Fri, Apr 26, 2024
Volume 7, Issue 2 (6-2018)
2018, 7(2): 85-93 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gholinia F, Dalili Kajan Z, Irannezhad A. Nonsurgical Miniscrew-Assisted Rapid Palatal Expansion in an Adult Patient. Journal title 2018; 7 (2) :85-93
URL: http://3dj.gums.ac.ir/article-1-319-en.html
URL: http://3dj.gums.ac.ir/article-1-319-en.html
1- Assistant Professor, Dental Sciences Research Center, Department of Orthodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
2- Professor, Dental Sciences Research Center, Department of Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Postgraduate Student, Department of Orthodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
2- Professor, Dental Sciences Research Center, Department of Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Postgraduate Student, Department of Orthodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
Keywords: Miniscrew-Assisted Rapid Palatal Expansion, Adult, Expansion, Cone-beam computed tomography
Full-Text [PDF 2964 kb]
(1685 Downloads)
| Abstract (HTML) (2262 Views)
Full-Text: (2682 Views)
1. Case Report
Transverse maxillary deficiency is relatively prevalent in orthodontic patients and Rapid Maxillary Expansion (RME) is an acceptable method for the correction of this problem. However, orthopedic maxillary expansion with conventional RME in adults has been considered either impossible or rarely successful. This is because the midpalatal suture and adjacent articulations initiate to fuse by late adolescence and become more rigid with age. Consequently, the conventional expansion technique usually results in failure or limited expansion, root resorption, buccal crown tipping, periodontal damages, soft tissue inflammation, ulcerations, and the instability of treatment outcomes in adults. The nonsurgical MARPE technique was introduced to overcome adverse dentoalveolar effects and enhance skeletal expansion potential [1-3].
2. History
A 20-year-old woman referred to the Department of Orthodontic, Guilan University of Medical Sciences for consultation and treatment. Her chief complaints were anterior jaw opening and teeth irregularity. The patient had no medical complications or a history of trauma.
Examination and clinical findings
The facial analysis revealed facial symmetry, nasal tip deviation and increased lower anterior facial height. Upper and lower dental midline were coincident in relation to the midsagittal plane. Intraoral clinical examination and dental casts analyses revealed a class II canine and molar relationship, transverse maxillary deficiency, and bilateral posterior crossbite. Maxillary and mandibular arch length discrepancies were 10 mm and 12 mm, respectively. Maxillary interpremolar width was 26 mm and intermolar width was 30 mm (Figure 1).
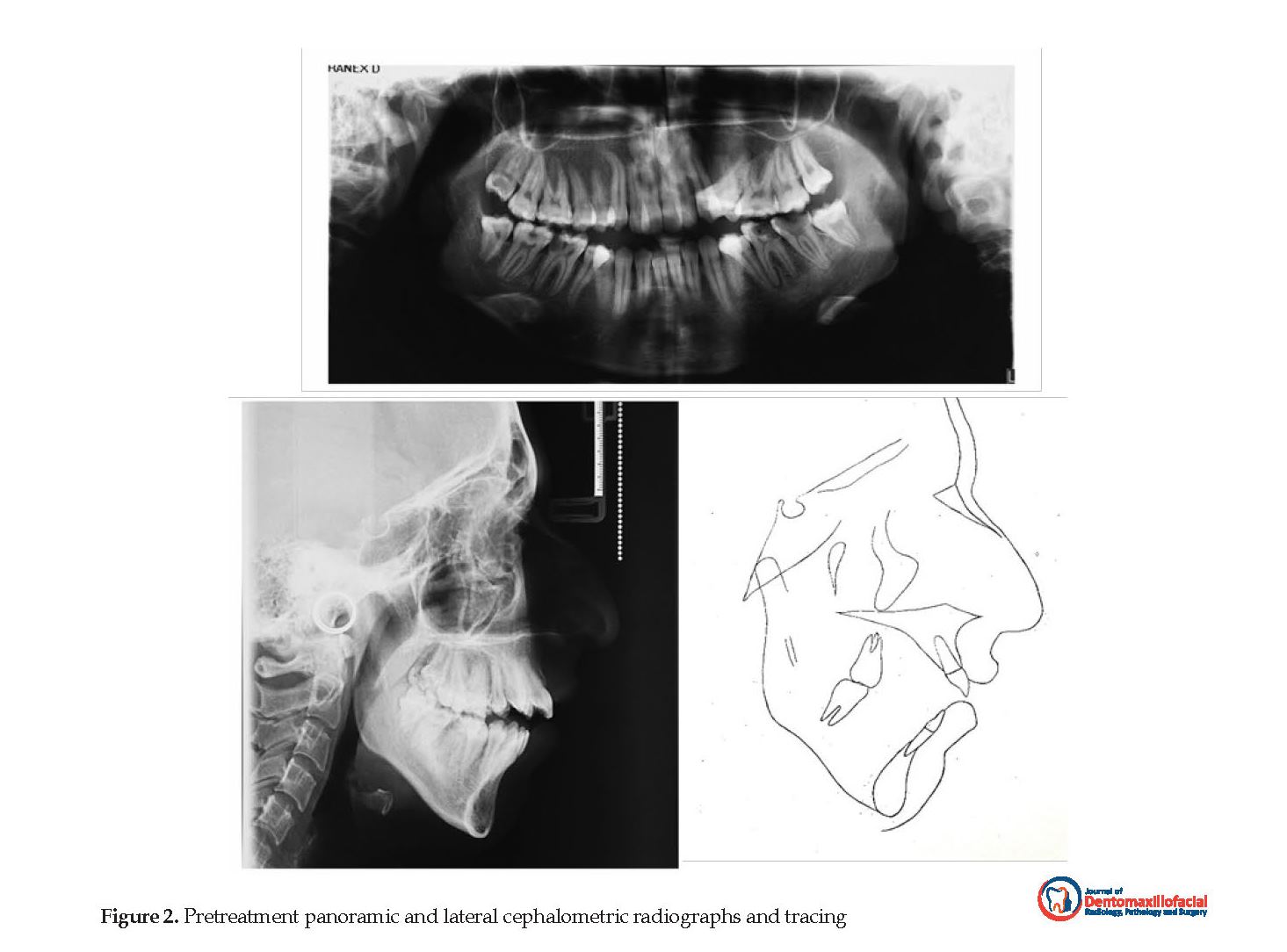
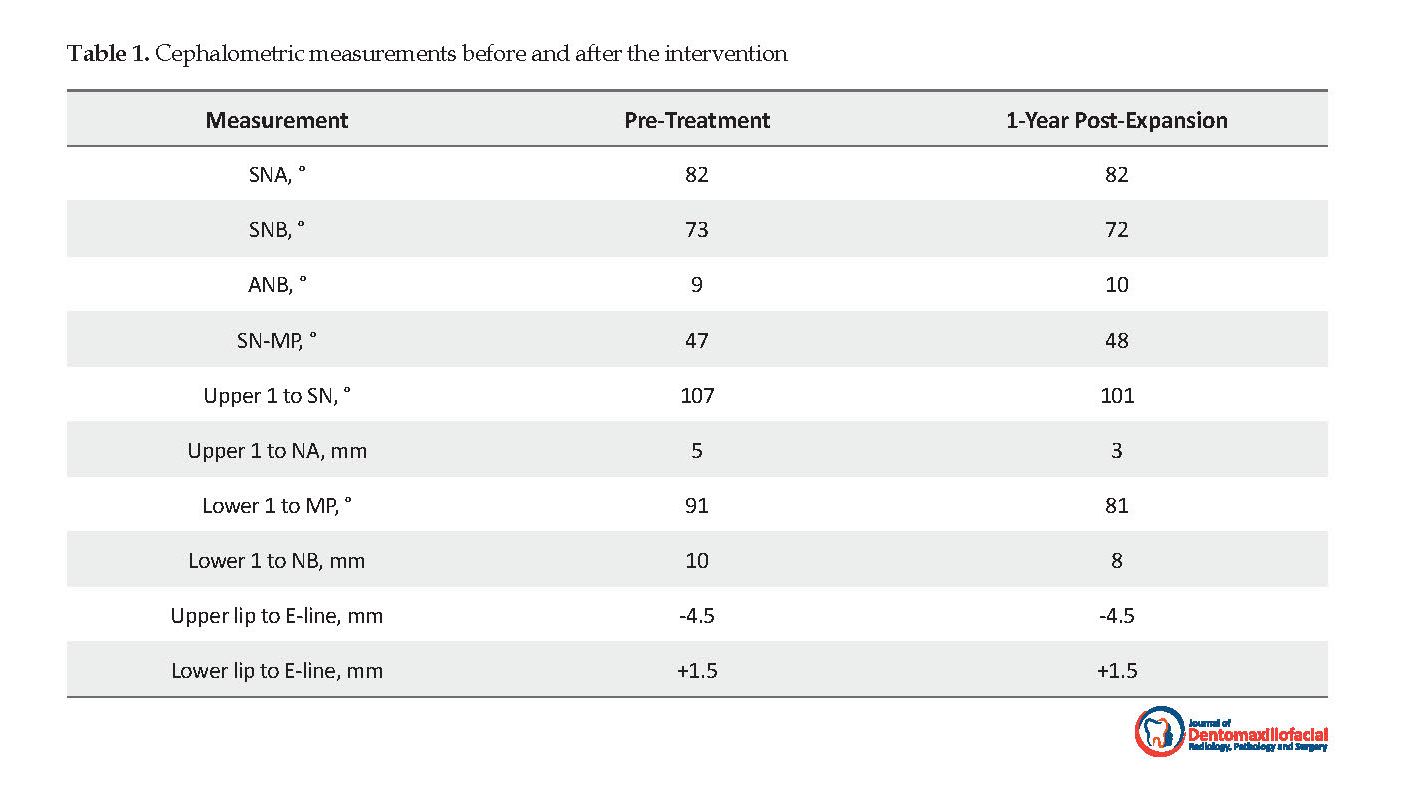
Radiographic analysis demonstrated deep caries with furcation involvement and bone resorption in mandibular right first molar and mandibular left first and second molars. After endodontic consultation, the extraction of these teeth was in order. The lateral cephalometric analysis suggested a class I rotated to class II skeletal pattern (ANB=9º), hyperdivergent facial planes (SN to MP=47º), proclined upper incisors (U1 to SN=107º), and well-positioned lower incisors (IMPA=91º) (Figure 2). After clinical examination, the patient was referred to an ENT specialist due to mouth breathing. In CBCT examination, the septal deviation and mucosal thickening of maxillary sinus were found.
3. Intervention
The treatment plan of the patient consisted of two phases. The first phase was a skeletal maxillary expansion to correct transverse maxillary deficiency explained earlier. The second phase was conducted following the orthognathic surgery (maxillary impaction, mandibular advancement, and genioplasty) to correct vertical and anteroposterior discrepancies. This patient had a very deep palate. There was no available Miniscrew-Assisted Rapid Palatal Expansion (MARPE) appliance to adapt it. For the fabrication of MARPE, the conventional Rapid Palatal Expansion (RPE) was modified based on Lee et al. report [1].
Transverse maxillary deficiency is relatively prevalent in orthodontic patients and Rapid Maxillary Expansion (RME) is an acceptable method for the correction of this problem. However, orthopedic maxillary expansion with conventional RME in adults has been considered either impossible or rarely successful. This is because the midpalatal suture and adjacent articulations initiate to fuse by late adolescence and become more rigid with age. Consequently, the conventional expansion technique usually results in failure or limited expansion, root resorption, buccal crown tipping, periodontal damages, soft tissue inflammation, ulcerations, and the instability of treatment outcomes in adults. The nonsurgical MARPE technique was introduced to overcome adverse dentoalveolar effects and enhance skeletal expansion potential [1-3].
2. History
A 20-year-old woman referred to the Department of Orthodontic, Guilan University of Medical Sciences for consultation and treatment. Her chief complaints were anterior jaw opening and teeth irregularity. The patient had no medical complications or a history of trauma.
Examination and clinical findings
The facial analysis revealed facial symmetry, nasal tip deviation and increased lower anterior facial height. Upper and lower dental midline were coincident in relation to the midsagittal plane. Intraoral clinical examination and dental casts analyses revealed a class II canine and molar relationship, transverse maxillary deficiency, and bilateral posterior crossbite. Maxillary and mandibular arch length discrepancies were 10 mm and 12 mm, respectively. Maxillary interpremolar width was 26 mm and intermolar width was 30 mm (Figure 1).
Radiographic analysis demonstrated deep caries with furcation involvement and bone resorption in mandibular right first molar and mandibular left first and second molars. After endodontic consultation, the extraction of these teeth was in order. The lateral cephalometric analysis suggested a class I rotated to class II skeletal pattern (ANB=9º), hyperdivergent facial planes (SN to MP=47º), proclined upper incisors (U1 to SN=107º), and well-positioned lower incisors (IMPA=91º) (Figure 2). After clinical examination, the patient was referred to an ENT specialist due to mouth breathing. In CBCT examination, the septal deviation and mucosal thickening of maxillary sinus were found.
3. Intervention
The treatment plan of the patient consisted of two phases. The first phase was a skeletal maxillary expansion to correct transverse maxillary deficiency explained earlier. The second phase was conducted following the orthognathic surgery (maxillary impaction, mandibular advancement, and genioplasty) to correct vertical and anteroposterior discrepancies. This patient had a very deep palate. There was no available Miniscrew-Assisted Rapid Palatal Expansion (MARPE) appliance to adapt it. For the fabrication of MARPE, the conventional Rapid Palatal Expansion (RPE) was modified based on Lee et al. report [1].
After the placement of bands on the first premolars and molars, an impression was made. Then, a conventional hyrax expander was fabricated on the plaster cast. The 4 rigid connectors of stainless steel wire (0.9 mm) with helical hooks were soldered on the base of screw. After evaluation of bone thickness on CBCT, two anterior and posterior hooks were located on the rugae region and parasagittal area, respectively. The hooks were adjusted for passive contact with the palate. The MARPE appliance was adjusted and cemented. After local anesthesia, 4 orthodontic miniscrews (1.8 mm diameter x 10 mm and 8 mm length, for anterior and posterior regions, respectively) (Dual Top Anchor System, Jeil Medical, Seoul, Korea) were located in the center of the hooks; then, covered by a light-cured composite (Transbond XT, 3M Unitek, Monrovia, California, USA). Figure 3 shows the used modification of the MARPE device.
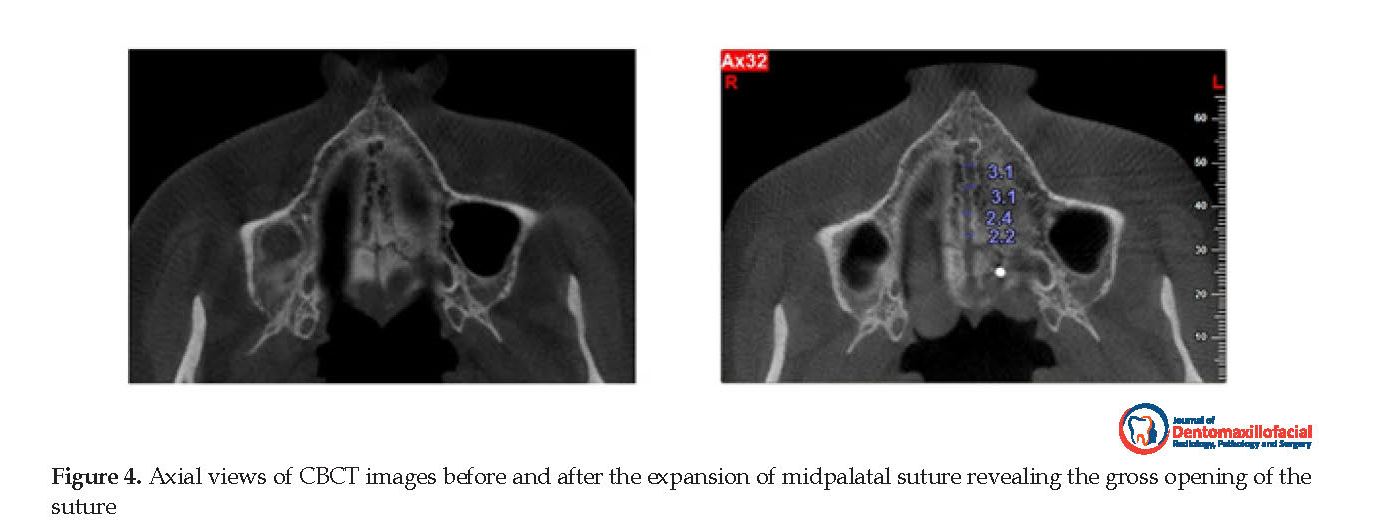
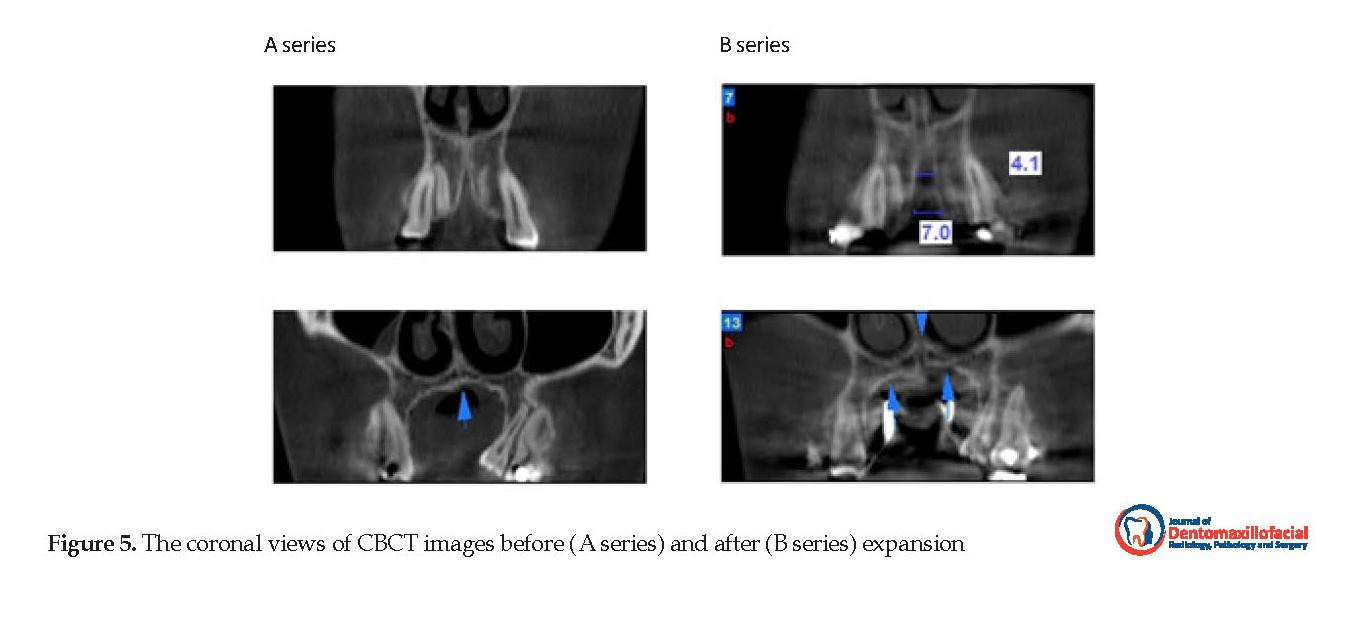
The activation protocol was one-quarter turn (0.2 mm) per day every other day, with the total activation duration of 10 weeks. After active expansion, for bone formation in the split palatal suture, the MARPE was maintained there for 3 months. After obtaining the informed consent from the patient, the disjunction of the midpalatal suture was confirmed with a CBCT. The axial view of the later CBCT in the level of Midpalatal Suture (MPS) was compared with the primary CBCT of the patient which was ordered by ENT specialist (Figures 4 and 5).
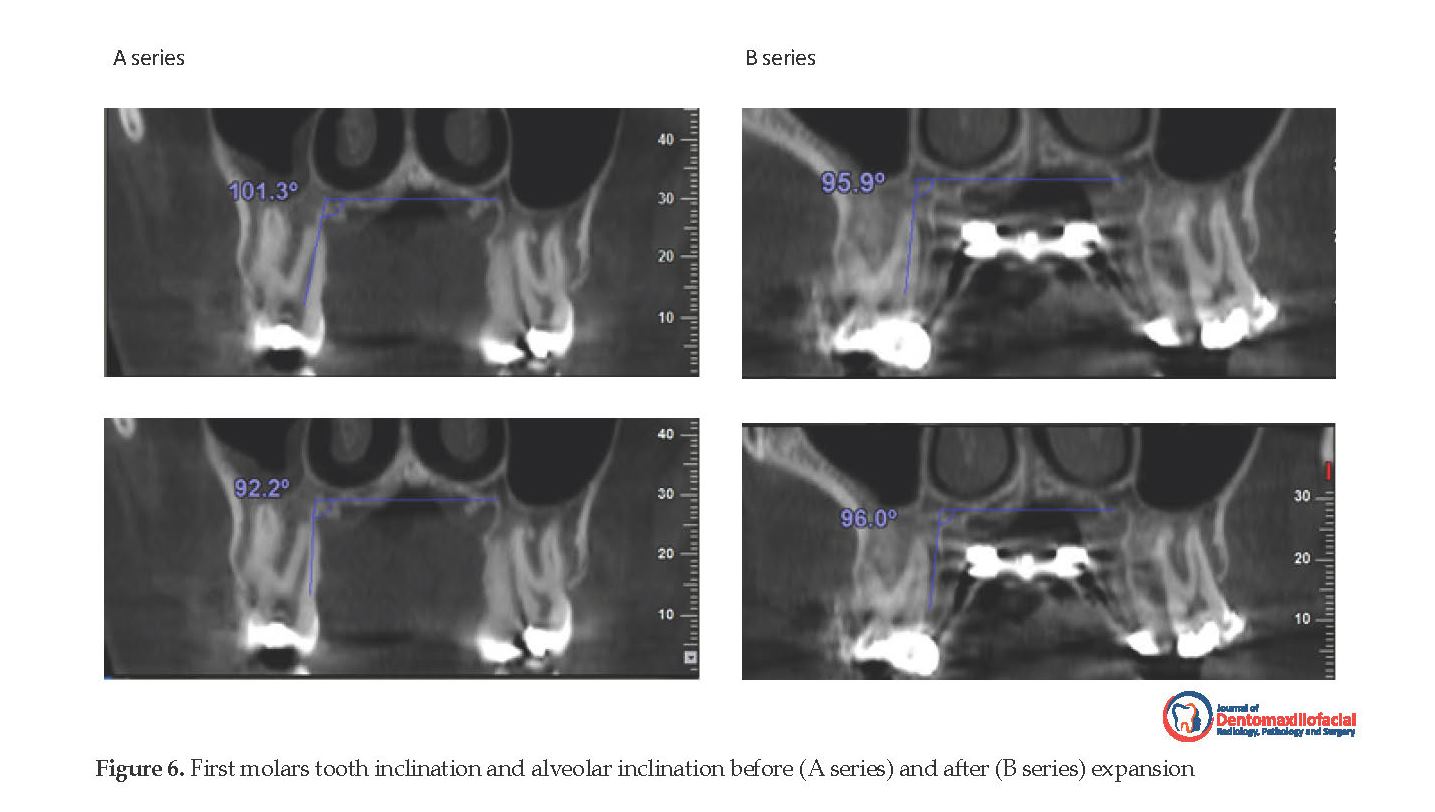
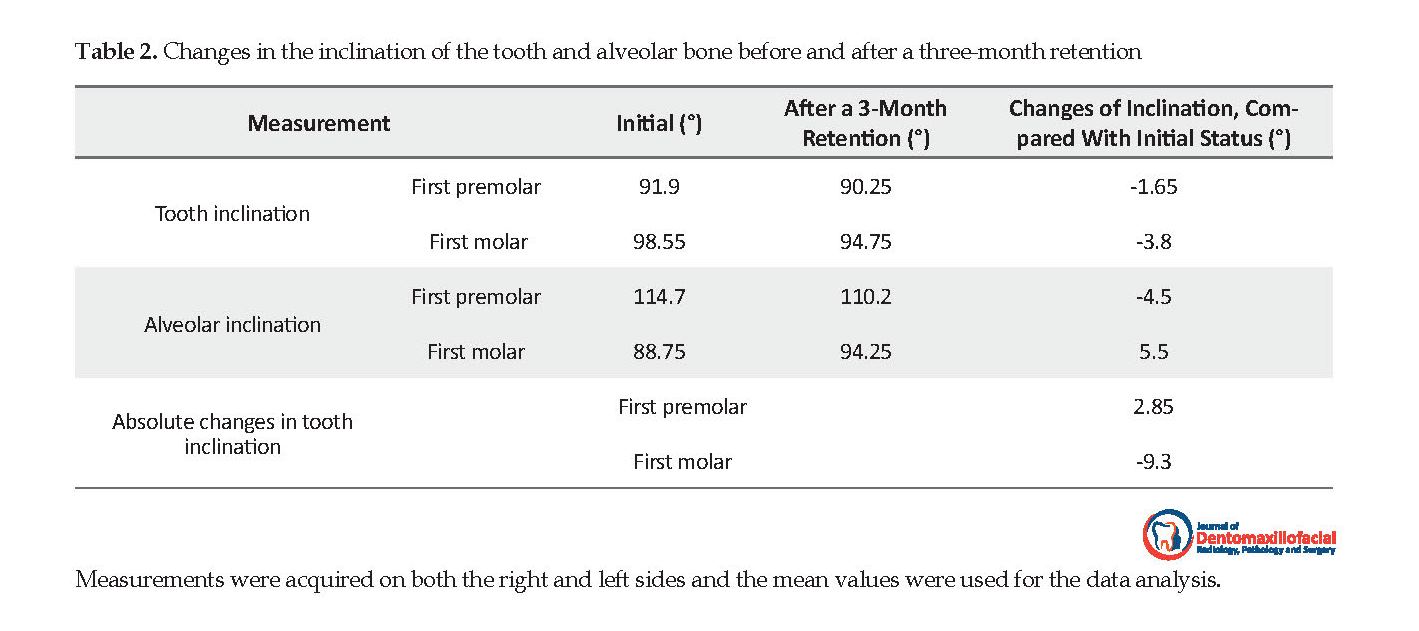
In addition, in a coronal section of CBCT passing through the centers of the first premolar and first molar palatal roots, the following measurements were recorded: tooth inclination, alveolar inclination, and absolute change in tooth inclination. Tooth inclination is defined as the angle between the long axis of the first premolar and first molar palatal root and the palatal plane. The alveolar inclination is defined as the angle between the palatal alveolar bone and the palatal plane. Absolute change in tooth inclination is defined as subtracting the alveolar inclination value from the tooth inclination value. For the evaluation of changes in inclination, measurements were performed on both sides (Figure 6), and the mean values were used for the data analysis [2].
4. Evaluation
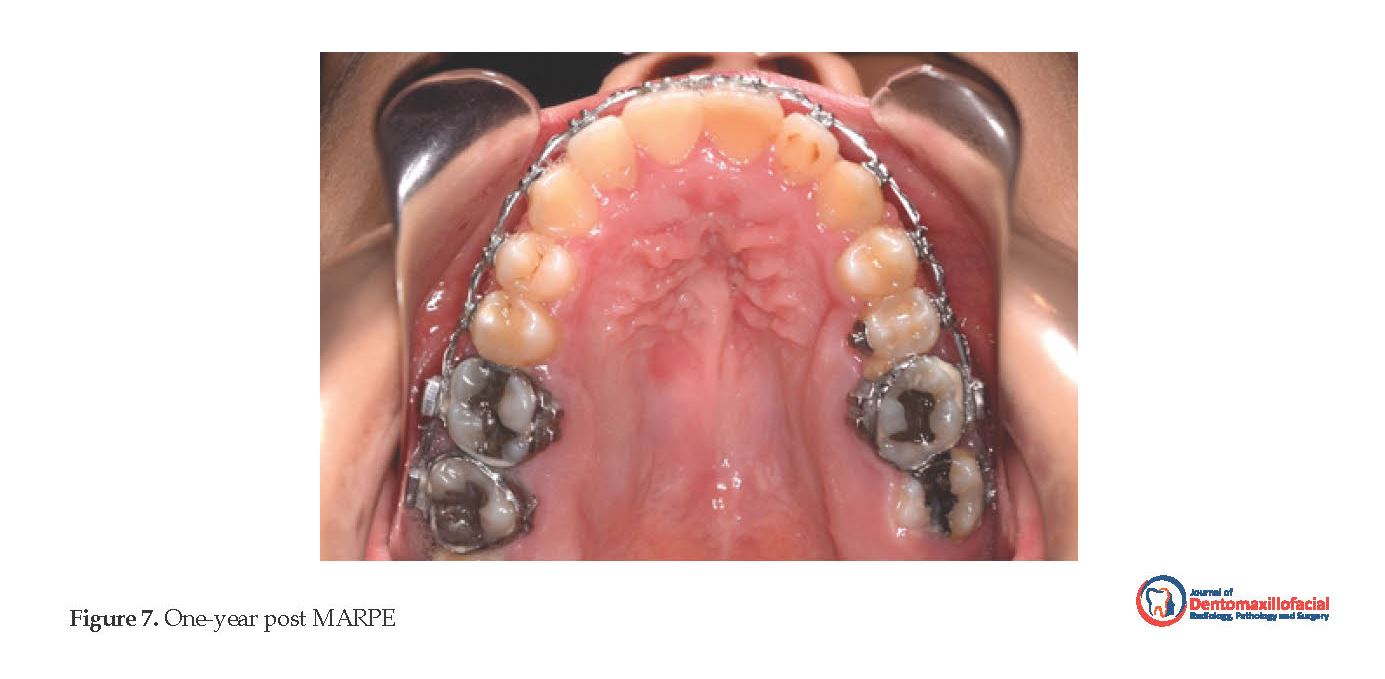
After the retention period, a removable Transpalatal arch (TPA) was placed in upper arch for the correction of the mesiolingual rotation of maxillary first molars. Figure 7 shows the one-year post-expansion status of the patient. Cephalometric outcomes indicated that the maxillary and mandibular incisors were retroclined; however, the skeletal relationships almost remained unchanged (Table 1). Comparing CBCT images before and after expansion, the splitting of midpalatal suture in anterior and posterior parts were 3.1 and 2.2, respectively. The maxillary transverse discrepancy was resolved with an increase of 6 mm and 9 mm in the first premolars and first molars widths, respectively.
In addition, in a coronal section of CBCT passing through the centers of the first premolar and first molar palatal roots, the following measurements were recorded: tooth inclination, alveolar inclination, and absolute change in tooth inclination. Tooth inclination is defined as the angle between the long axis of the first premolar and first molar palatal root and the palatal plane. The alveolar inclination is defined as the angle between the palatal alveolar bone and the palatal plane. Absolute change in tooth inclination is defined as subtracting the alveolar inclination value from the tooth inclination value. For the evaluation of changes in inclination, measurements were performed on both sides (Figure 6), and the mean values were used for the data analysis [2].
4. Evaluation
After the retention period, a removable Transpalatal arch (TPA) was placed in upper arch for the correction of the mesiolingual rotation of maxillary first molars. Figure 7 shows the one-year post-expansion status of the patient. Cephalometric outcomes indicated that the maxillary and mandibular incisors were retroclined; however, the skeletal relationships almost remained unchanged (Table 1). Comparing CBCT images before and after expansion, the splitting of midpalatal suture in anterior and posterior parts were 3.1 and 2.2, respectively. The maxillary transverse discrepancy was resolved with an increase of 6 mm and 9 mm in the first premolars and first molars widths, respectively.
The first molars inclination decreased by 3.8º, while its corresponding alveolar inclination increased 5.5º, indicating a 9.3º uprighting of the tooth itself. In the first premolars area, the tooth and alveolar inclination decreased by 1.65º and 4.5º, respectively, indicating a slight buccal tipping of the tooth (Table 2). Using MARPE, the desired buccal segment occlusion and acceptable nonsurgical expansion of the maxilla were accomplished. Moreover, the periodontal condition remained stable after expansion. Proper facial esthetics result from the orthognathic surgery, as the next phase of treatment.
5. Discussion
Applying RPE in younger patients has been frequently supported by the literature. Moreover, palatal expansion has been reported to be less successful in nongrowing patients due to the maturation of the midpalatal suture and adjacent articulations. This in turn leads to higher resistance to mechanical forces [3]. CT and CBCT studies indicated that bone dehiscence, the reduction of alveolar bone height and thickness, post-expansion relapse, gingival recession and tipping and the bodily movement of anchor teeth might be the results of tooth tissue-borne (Haas type) or tooth-borne (Hyrax type) expanders. The higher risks of expansion have been reported in postpubertal patients. In addition, the stronger bone-borne anchorage is more required, compared to conventional expanders [4].
5. Discussion
Applying RPE in younger patients has been frequently supported by the literature. Moreover, palatal expansion has been reported to be less successful in nongrowing patients due to the maturation of the midpalatal suture and adjacent articulations. This in turn leads to higher resistance to mechanical forces [3]. CT and CBCT studies indicated that bone dehiscence, the reduction of alveolar bone height and thickness, post-expansion relapse, gingival recession and tipping and the bodily movement of anchor teeth might be the results of tooth tissue-borne (Haas type) or tooth-borne (Hyrax type) expanders. The higher risks of expansion have been reported in postpubertal patients. In addition, the stronger bone-borne anchorage is more required, compared to conventional expanders [4].
In adults, the surgical osteotomies may be used for maxillary skeletal expansion; however, arch width stability remains controversial. Phillips et al. reported remarkable relapse after expansion with Le Fort I and segmental osteotomy in 39 patients [5]. The SARPE yields demonstrated greater stability, compared with segmental osteotomy since those permit tissue adaptation during the expansion and consolidation phase [6, 7]. Berger et al. reported a non-significant difference of 1-year stability between SARPE in postpubertal patients, and nonsurgical expansion in prepubertal patients [8]. Thus, when the orthopedic expansion is achievable, the treatment outcomes and the stability of nonsurgical expansion are comparable with SARPE in adults.
Accordingly, the MARPE technique which is based on a tooth- and -bone-borne device was considered as an appropriate possibility for this adult case. By a miniscrew anchorage system, expansion forces are transmitted to basal bones resulting in higher skeletal expansion and sufficient structural stiffness as well as preserving the amount of expansion during the consolidation phase.
This case illustrates an efficacious maxillary expansion in an adult with type I palatal split pattern. It indicates a complete disjunction of the midpalatal suture from the anterior- to posterior nasal spine. Furthermore, an incomplete disjunction of the midpalatal suture has been detected in the evaluation of SARPE technique, represented as type II palatal split pattern [9]. The achieved type I palatal split pattern by MARPE in the lack of any surgical osteotomy, suggests that the position of posterior miniscrews might significantly impact supplying sufficient stress distribution for the complete disjunction of the midpalatal suture.
The consensus is that palatal expansion success is mainly related to age; this is based on the idea that after the early teens, palatal expansion rapidly becomes inefficient [10]. Thus, the only choice for orthopedic expansion after adolescence was surgery. Nevertheless, the validity of nonsurgical or surgical treatment should be reassessed in respect of safety, stability, and possibility. Opposing to the strong belief in adult patients that nonsurgical palatal expansion is impractical, a clear skeletal expansion was detected after the treatment of our patient. This data was confirmed by exact measurements and comparisons based on CBCT images. As the appliance is tooth- and bone-borne, the treatment effects can be described as a combination of skeletal and dentoalveolar expansions.
The patients’ post-expansion outcomes revealed that the major buccal tipping of the teeth was controlled. This is because of the rigid frame, and the force designed to be exerted through the miniscrews on the bone before affecting the teeth. Evaluating the coronal images of the first premolars and first molars suggested that the alveolar inclination changes were greater than the tooth inclination changes. Accordingly, the first premolars were slightly buccaly and the first molars were a little upright.
Lee et al. treated a 20-year-old patient with mandibular prognathism and severe transverse deficiency. Before conducting the orthognathic surgery, MARPE appliance was used. The separation of midpalatal suture was confirmed with intraoral radiographs and a posteroanterior cephalogram. The intercanine and intermolar widths increased 2.7 mm and 8.3 mm, respectively. Based on the evaluation of dental casts, only minimal change occurred in buccolingual molar inclination. The minimal damage to teeth and periodontium, with stable outcomes, was achieved with expansion and confirmed by clinical and two-dimensional radiographic evaluations. They concluded that MARPE was an effective treatment method to improve transverse discrepancies and applying surgical techniques in such patients might be unnecessary [1].
Cunha et al. described the non-extraction treatment of a 24-year-old woman with MARPE appliance. Their outcomes revealed the interpremolar and the intermolar widths increased 7.8 mm and 5 mm, respectively. Moreover, the mid palatal suture splitting in anterior, intermediate and posterior midpalate were 4.9 mm, 3.6 mm, and 2.4 mm, respectively. They stated MARPE is effective in transverse problems and should be considered as an alternative for the management of arch perimeter in adults [11].
Carlson et al. employed a prefabricated MARPE appliance in a 19-year-old man with maxillary constriction. In their study, the intercanine and intermolar widths increased 7.0 mm and 6.0 mm, respectively. Expansion at midpalatal suture was 3.8 mm. In addition, the first molars and premolars revealed a slight increase in buccolingual angulation in CBCT assessment [12].
Park et al. studied post-MARPE skeletal and dentoalveolar changes using CBCT in 14 patients with the mean age of 20.1 years. The midpalatal suture was separate and the maxilla indicated significant lateral movement. The interpremolar and intermolar widths increased 5.5 mm and 5.4 mm, respectively. The premolars and molars showed the buccal tipping of 1.1º to 2.9º. They concluded MARPE is a successful approach for solving maxillary transverse problems without conducting surgery in adults [13].
Lim et al. assessed the post-MARPE stability of dental, alveolar and skeletal changes in 24 patients with the mean age of 21.6 years. From before to immediately after conducting MARPE, interpremolar and intermolar widths increased 5.96 mm and 5.63 mm, respectively. Additionally, first molar revealed a 2.07º buccal tipping. Their results suggested that MARPE is effective for correcting transverse discrepancies, presenting stable outcomes one year after expansion [2].
Choi et al. assessed MARPE outcomes in 20 patients with the mean age of 20.9 years, using posteroanterior cephalometric records and dental casts. Suture separation was observed in 86.96% of the subjects. Interpremolar and intermolar widths increased 6.09 mm and 8.32 mm, respectively from the initial examination to post-MARPE removal. Their results indicated that MARPE is an appropriate method for the correction of the transverse maxillary problem in young adults [14].
In this case, we used a slow expansion protocol, with the activation of one-quarter turn per day every other day. The major objective was permitting sufficient tissues adaptation to applied forces and minimizing patient’s discomfort, mainly because of increased maxillary bone stiffness with age.
We would like to indicate the special importance of our case report due to the following reasons: 1. MARPE was used in an adult patient; 2. Because of the patient’s very deep palate and difficulty of adapting prefabricated appliances, we designed a custom-made appliance which is a low-cost version of MARPE; 3. Large skeletal effects on the maxillary width was demonstrated; and 4. CBCT was used to improve the examination and evaluation of treatment outcomes.
6. Conclusion
This case report reveals the successful treatment of a mature patient with severe maxillary constriction and very deep palate with a posterior crossbite using a custom-made modification of MARPE. Because of lower costs and fewer complications, compared to other treatment alternatives, this MARPE design and protocol hold considerable promise for the perspective of nonsurgical orthopedic expansion in adults. Obviously, additional studies should be conducted to prove the efficiency of this treatment modality in various demographic group of patients. In addition, this report assessed the short-term retention of the expansion phase of treatment; thus, for long-term evaluations, the patient should be followed-up in the future.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participant was informed about the purpose of the research and its implementation stages; she was also assured about the confidentiality of her information; Moreover, She was allowed to leave the study whenever she wish, and if desired, the results of the research would be available to her.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, Methodology, Writing-Review, Editing and supervision: Faegheh Gholinia, Zahra Dalili Kajan; and Methodology, Software, Resources, Writing-original draft preparation, Writing-review: Azin Irannezhad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank the staff of the Department of Orthodontics in the Dental School of Guilan University of Medical Sciences, for their contribution in the current research.
References
Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. American Journal of Orthodontics and Dentofacial Orthopedics. 2010; 137(6):830-9. [DOI:10.1016/j.ajodo.2007.10.065] [PMID]
Lim HM, Park YC, Lee KJ, Kim KH, Choi YJ. S ility of dental, alveolar, and skeletal changes after Miniscrew-Assisted Rapid Palatal Expansion. The Korean Journal of Orthodontics. 2017; 47(5):313-22. [DOI:10.4041/kjod.2017.47.5.313] [PMID] [PMCID]
Melsen B, Melsen F. The postnatal development of the palatomaxillary region studied on human autopsy material. American Journal of Orthodontics and Dentofacial Orthopedics. 1982; 82(4):329-42. [DOI:10.1016/0002-9416(82)90467-5]
Garib DG, Henriques JF, Janson G, Freitas MR, Fernandes AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: A computed tomography evaluation. American Journal of Orthodontics and Dentofacial Orthopedics. 2006; 129(6):749-58. [DOI:10.1016/j.ajodo.2006.02.021] [PMID]
Phillips C, Medland WH, Fields HW Jr, Proffit WR, White RP Jr. Stability of surgical maxillary expansion. The International Journal of Adult Orthodontics & Orthognathic Surgery. 1992; 7(3):139-46. [PMID]
Koudstaal MJ, Poort LJ, van der Wal KG, Wolvius EB, Prahl-Andersen B, Schulten AJ. Surgically Assisted Rapid Maxillary Expansion (SARME): A review of the literature. International Journal of Oral and Maxillofacial Surgery. 2005; 34(7):709-14. [DOI:10.1016/j.ijom.2005.04.025] [PMID]
Bailey LJ, White RP Jr, Proffit WR, Turvey TA. Segmental LeFort I osteotomy for management of transverse maxillary deficiency. Journal of Oral and Maxillofacial Surgery. 1997; 55(7):728-31. [DOI:10.1016/S0278-2391(97)90588-7]
Berger JL, Pangrazio-KulbershV, Borgula T, Kaczynski R. Stability of orthopedic and surgically assisted rapid palatal expansion over time. American Journal of Orthodontics and Dentofacial Orthopedics. 1998; 114(6):638-45. [DOI:10.1016/S0889-5406(98)70195-7]
Pereira MD, Prado GP, Abramoff mm, Aloise AC, Masako Ferreira L. Classification of midpalatal suture opening after surgically assisted rapid maxillary expansion using computed tomography. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2010; 110(1):41-5. [DOI:10.1016/j.tripleo.2009.12.028] [PMID]
Handelman CS. Nonsurgical rapid maxillary alveolar expansion in adults: A clinical evaluation. The Angle Orthodontist. 1997; 67(4):291-308. [DOI: 10.1043/0003-3219(1997)067<0291:NRMAEI>2.3.CO;2] [PMID]
Cunha ACD, Lee H, Nojima LI, Nojima MDCG, Lee KJ. Miniscrew-Assisted Rapid Palatal Expansion for managing arch perimeter in an adult patient. Dental Press Journal of Orthodontics. 2017; 22(3):97-108. [DOI:10.1590/2177-6709.22.3.097-108.oar] [PMID] [PMCID]
Carlson C, Sung J, McComb RW, Machado AW, Moon W. Microimplant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. American Journal of Orthodontics and Dentofacial Orthopedics. 2016; 149(5):716-28. [DOI:10.1016/j.ajodo.2015.04.043] [PMID]
Park JJ, Park YC, Lee KJ, Cha JY, Tahk JH, Choi YJ. Skeletal and dentoalveolar changes after Miniscrew-Assisted Rapid Palatal Expansion in young adults: A cone-beam computed tomography study. The Korean Journal of Orthodontics. 2017; 47(2):77-86. [DOI:10.4041/kjod.2017.47.2.77]
Choi SH, Shi KK, Cha JY, Park YC, Lee KJ. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. The Angle Orthodontist. 2016; 86(5):713-20. [DOI:10.2319/101415-689.1] [PMID]
The consensus is that palatal expansion success is mainly related to age; this is based on the idea that after the early teens, palatal expansion rapidly becomes inefficient [10]. Thus, the only choice for orthopedic expansion after adolescence was surgery. Nevertheless, the validity of nonsurgical or surgical treatment should be reassessed in respect of safety, stability, and possibility. Opposing to the strong belief in adult patients that nonsurgical palatal expansion is impractical, a clear skeletal expansion was detected after the treatment of our patient. This data was confirmed by exact measurements and comparisons based on CBCT images. As the appliance is tooth- and bone-borne, the treatment effects can be described as a combination of skeletal and dentoalveolar expansions.
The patients’ post-expansion outcomes revealed that the major buccal tipping of the teeth was controlled. This is because of the rigid frame, and the force designed to be exerted through the miniscrews on the bone before affecting the teeth. Evaluating the coronal images of the first premolars and first molars suggested that the alveolar inclination changes were greater than the tooth inclination changes. Accordingly, the first premolars were slightly buccaly and the first molars were a little upright.
Lee et al. treated a 20-year-old patient with mandibular prognathism and severe transverse deficiency. Before conducting the orthognathic surgery, MARPE appliance was used. The separation of midpalatal suture was confirmed with intraoral radiographs and a posteroanterior cephalogram. The intercanine and intermolar widths increased 2.7 mm and 8.3 mm, respectively. Based on the evaluation of dental casts, only minimal change occurred in buccolingual molar inclination. The minimal damage to teeth and periodontium, with stable outcomes, was achieved with expansion and confirmed by clinical and two-dimensional radiographic evaluations. They concluded that MARPE was an effective treatment method to improve transverse discrepancies and applying surgical techniques in such patients might be unnecessary [1].
Cunha et al. described the non-extraction treatment of a 24-year-old woman with MARPE appliance. Their outcomes revealed the interpremolar and the intermolar widths increased 7.8 mm and 5 mm, respectively. Moreover, the mid palatal suture splitting in anterior, intermediate and posterior midpalate were 4.9 mm, 3.6 mm, and 2.4 mm, respectively. They stated MARPE is effective in transverse problems and should be considered as an alternative for the management of arch perimeter in adults [11].
Carlson et al. employed a prefabricated MARPE appliance in a 19-year-old man with maxillary constriction. In their study, the intercanine and intermolar widths increased 7.0 mm and 6.0 mm, respectively. Expansion at midpalatal suture was 3.8 mm. In addition, the first molars and premolars revealed a slight increase in buccolingual angulation in CBCT assessment [12].
Park et al. studied post-MARPE skeletal and dentoalveolar changes using CBCT in 14 patients with the mean age of 20.1 years. The midpalatal suture was separate and the maxilla indicated significant lateral movement. The interpremolar and intermolar widths increased 5.5 mm and 5.4 mm, respectively. The premolars and molars showed the buccal tipping of 1.1º to 2.9º. They concluded MARPE is a successful approach for solving maxillary transverse problems without conducting surgery in adults [13].
Lim et al. assessed the post-MARPE stability of dental, alveolar and skeletal changes in 24 patients with the mean age of 21.6 years. From before to immediately after conducting MARPE, interpremolar and intermolar widths increased 5.96 mm and 5.63 mm, respectively. Additionally, first molar revealed a 2.07º buccal tipping. Their results suggested that MARPE is effective for correcting transverse discrepancies, presenting stable outcomes one year after expansion [2].
Choi et al. assessed MARPE outcomes in 20 patients with the mean age of 20.9 years, using posteroanterior cephalometric records and dental casts. Suture separation was observed in 86.96% of the subjects. Interpremolar and intermolar widths increased 6.09 mm and 8.32 mm, respectively from the initial examination to post-MARPE removal. Their results indicated that MARPE is an appropriate method for the correction of the transverse maxillary problem in young adults [14].
In this case, we used a slow expansion protocol, with the activation of one-quarter turn per day every other day. The major objective was permitting sufficient tissues adaptation to applied forces and minimizing patient’s discomfort, mainly because of increased maxillary bone stiffness with age.
We would like to indicate the special importance of our case report due to the following reasons: 1. MARPE was used in an adult patient; 2. Because of the patient’s very deep palate and difficulty of adapting prefabricated appliances, we designed a custom-made appliance which is a low-cost version of MARPE; 3. Large skeletal effects on the maxillary width was demonstrated; and 4. CBCT was used to improve the examination and evaluation of treatment outcomes.
6. Conclusion
This case report reveals the successful treatment of a mature patient with severe maxillary constriction and very deep palate with a posterior crossbite using a custom-made modification of MARPE. Because of lower costs and fewer complications, compared to other treatment alternatives, this MARPE design and protocol hold considerable promise for the perspective of nonsurgical orthopedic expansion in adults. Obviously, additional studies should be conducted to prove the efficiency of this treatment modality in various demographic group of patients. In addition, this report assessed the short-term retention of the expansion phase of treatment; thus, for long-term evaluations, the patient should be followed-up in the future.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participant was informed about the purpose of the research and its implementation stages; she was also assured about the confidentiality of her information; Moreover, She was allowed to leave the study whenever she wish, and if desired, the results of the research would be available to her.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, Methodology, Writing-Review, Editing and supervision: Faegheh Gholinia, Zahra Dalili Kajan; and Methodology, Software, Resources, Writing-original draft preparation, Writing-review: Azin Irannezhad.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We would like to thank the staff of the Department of Orthodontics in the Dental School of Guilan University of Medical Sciences, for their contribution in the current research.
References
Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. American Journal of Orthodontics and Dentofacial Orthopedics. 2010; 137(6):830-9. [DOI:10.1016/j.ajodo.2007.10.065] [PMID]
Lim HM, Park YC, Lee KJ, Kim KH, Choi YJ. S ility of dental, alveolar, and skeletal changes after Miniscrew-Assisted Rapid Palatal Expansion. The Korean Journal of Orthodontics. 2017; 47(5):313-22. [DOI:10.4041/kjod.2017.47.5.313] [PMID] [PMCID]
Melsen B, Melsen F. The postnatal development of the palatomaxillary region studied on human autopsy material. American Journal of Orthodontics and Dentofacial Orthopedics. 1982; 82(4):329-42. [DOI:10.1016/0002-9416(82)90467-5]
Garib DG, Henriques JF, Janson G, Freitas MR, Fernandes AY. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: A computed tomography evaluation. American Journal of Orthodontics and Dentofacial Orthopedics. 2006; 129(6):749-58. [DOI:10.1016/j.ajodo.2006.02.021] [PMID]
Phillips C, Medland WH, Fields HW Jr, Proffit WR, White RP Jr. Stability of surgical maxillary expansion. The International Journal of Adult Orthodontics & Orthognathic Surgery. 1992; 7(3):139-46. [PMID]
Koudstaal MJ, Poort LJ, van der Wal KG, Wolvius EB, Prahl-Andersen B, Schulten AJ. Surgically Assisted Rapid Maxillary Expansion (SARME): A review of the literature. International Journal of Oral and Maxillofacial Surgery. 2005; 34(7):709-14. [DOI:10.1016/j.ijom.2005.04.025] [PMID]
Bailey LJ, White RP Jr, Proffit WR, Turvey TA. Segmental LeFort I osteotomy for management of transverse maxillary deficiency. Journal of Oral and Maxillofacial Surgery. 1997; 55(7):728-31. [DOI:10.1016/S0278-2391(97)90588-7]
Berger JL, Pangrazio-KulbershV, Borgula T, Kaczynski R. Stability of orthopedic and surgically assisted rapid palatal expansion over time. American Journal of Orthodontics and Dentofacial Orthopedics. 1998; 114(6):638-45. [DOI:10.1016/S0889-5406(98)70195-7]
Pereira MD, Prado GP, Abramoff mm, Aloise AC, Masako Ferreira L. Classification of midpalatal suture opening after surgically assisted rapid maxillary expansion using computed tomography. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2010; 110(1):41-5. [DOI:10.1016/j.tripleo.2009.12.028] [PMID]
Handelman CS. Nonsurgical rapid maxillary alveolar expansion in adults: A clinical evaluation. The Angle Orthodontist. 1997; 67(4):291-308. [DOI: 10.1043/0003-3219(1997)067<0291:NRMAEI>2.3.CO;2] [PMID]
Cunha ACD, Lee H, Nojima LI, Nojima MDCG, Lee KJ. Miniscrew-Assisted Rapid Palatal Expansion for managing arch perimeter in an adult patient. Dental Press Journal of Orthodontics. 2017; 22(3):97-108. [DOI:10.1590/2177-6709.22.3.097-108.oar] [PMID] [PMCID]
Carlson C, Sung J, McComb RW, Machado AW, Moon W. Microimplant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. American Journal of Orthodontics and Dentofacial Orthopedics. 2016; 149(5):716-28. [DOI:10.1016/j.ajodo.2015.04.043] [PMID]
Park JJ, Park YC, Lee KJ, Cha JY, Tahk JH, Choi YJ. Skeletal and dentoalveolar changes after Miniscrew-Assisted Rapid Palatal Expansion in young adults: A cone-beam computed tomography study. The Korean Journal of Orthodontics. 2017; 47(2):77-86. [DOI:10.4041/kjod.2017.47.2.77]
Choi SH, Shi KK, Cha JY, Park YC, Lee KJ. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. The Angle Orthodontist. 2016; 86(5):713-20. [DOI:10.2319/101415-689.1] [PMID]
Received: 2018/01/2 | Accepted: 2018/04/28 | Published: 2018/06/1
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |