Sat, May 4, 2024
Volume 6, Issue 3 (10-2017)
2017, 6(3): 83-88 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nemati S, Sohrabi M, Dalili Kajan Z, Yousefi Z. Anterior Variant of Lingual Salivary Gland Depression: Review and A Case Report. Journal title 2017; 6 (3) :83-88
URL: http://3dj.gums.ac.ir/article-1-284-en.html
URL: http://3dj.gums.ac.ir/article-1-284-en.html
1- Assistant Professor, Dental Science Research Center, Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
2- Oral and Maxillofacial Radiologist, Private Clinic, Mashhad, Iran.
3- Professor, Dental Science Research Center, Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
4- Postgraduate Student of Dentomaxillofacial Radiology, Dental Science Research Center, Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. , Zahra_yousefi_sh@yahoo.com
2- Oral and Maxillofacial Radiologist, Private Clinic, Mashhad, Iran.
3- Professor, Dental Science Research Center, Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
4- Postgraduate Student of Dentomaxillofacial Radiology, Dental Science Research Center, Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. , Zahra_yousefi_sh@yahoo.com
Full-Text [PDF 987 kb]
(1061 Downloads)
| Abstract (HTML) (3487 Views)
Full-Text: (1990 Views)
1. Case Report
A 42-year-old male was referred to our private Oral and Maxillofacial Radiology Clinic for Cone-Beam Computed Tomography (CBCT) imaging of the mandible to examine the left mandibular cuspid (canine).
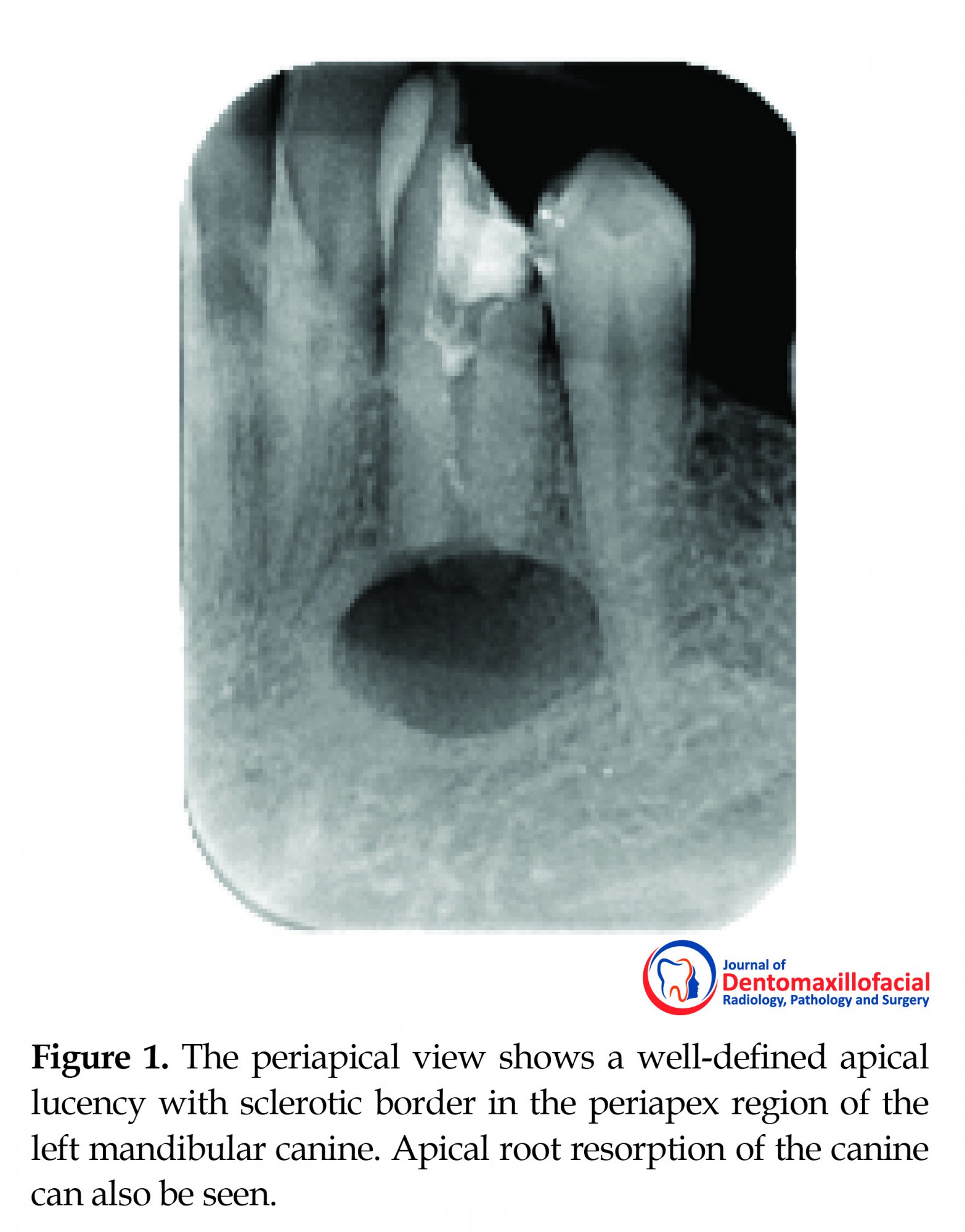
The Periapical (PA) view showed a well-defined apical lucency with a sclerotic border in the periapex region of the left mandibular canine (Figure 1). Apical root resorption of the canine was seen. On dental examination, the canine was found to have necrosis and required root canal therapy. Based on PA radiographic findings, the lesion mimicked a radicular cyst; this diagnosis was also supported by the necrosis of the canine. For further examination, the CBCT images were prepared by using the Planmeca CBCT device having a field of view of 10×6 cm, 12.5 mA, 90 Kvp, 0.5-mm slice thickness, and 1-mm slice distance.
A 42-year-old male was referred to our private Oral and Maxillofacial Radiology Clinic for Cone-Beam Computed Tomography (CBCT) imaging of the mandible to examine the left mandibular cuspid (canine).
The Periapical (PA) view showed a well-defined apical lucency with a sclerotic border in the periapex region of the left mandibular canine (Figure 1). Apical root resorption of the canine was seen. On dental examination, the canine was found to have necrosis and required root canal therapy. Based on PA radiographic findings, the lesion mimicked a radicular cyst; this diagnosis was also supported by the necrosis of the canine. For further examination, the CBCT images were prepared by using the Planmeca CBCT device having a field of view of 10×6 cm, 12.5 mA, 90 Kvp, 0.5-mm slice thickness, and 1-mm slice distance.
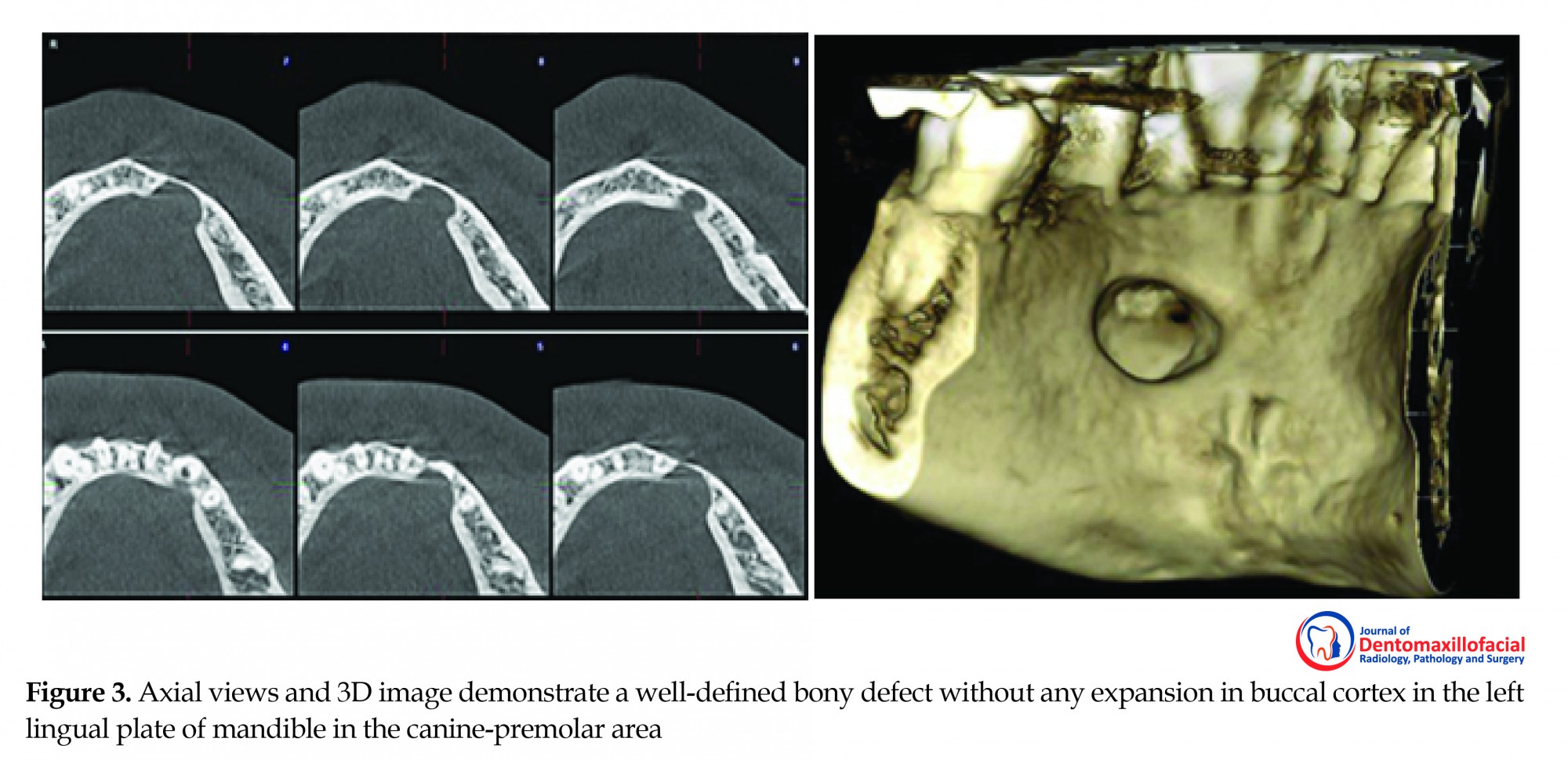
The cross-sectional (Figure 2), axial, and 3D images (Figure 3) revealed a bony defect with a well-defined corticated border in the lingual aspect of the mandible adjacent to the left mandibular canine. This remarkable finding was root resorption of the left mandibular canine. The possibility of surgical defect due to intact buccal cortex was ruled out.
In differential diagnosis, an anterior variant of the lingual salivary gland depression was considered. Root resorption of the left mandibular canine was justified due to necrosis and pulpoperiapical origin as an independent cause.
2. Discussion
Lingual mandibular bone depression represents a group of cavities in the lingual surface of the mandible while they have intact outer cortex. Historically, they were referred to as pseudocysts because they resemble a cyst in radiographic examination. It should be noted here that they are not true cysts because no epithelial lining is present in histology [1].
These defects were first introduced by Edward Stafne in 1942 [2]. He described these defects as asymptomatic and well-defined radiolucent cavities that were unilaterally located in the posterior region of the mandible between the mandibular angle and the third molar below the inferior dental canal. In his words, these defects were “bone cavities situated near the angle of the mandible” [3-8]. This asymptomatic defect is more likely to occur in men with a ratio of 6:1 and is usually observed at the age of over 40 years [5, 7, 9, 10].
These cavities are also known as lingual mandibular bone depression, developmental salivary gland defect, stafne defect, Stafne Bone Cyst (SBC), static bone cavity, latent bone cyst, and idiopathic bone cavity [1, 6].
Ariji et al. used CBCT to classify SBCs according to the depth of the cavity, as shown below: Type I: Cavity depth is limited to the medullar portion of the mandible; Type II: Cavity depth reaches the buccal cortex of the mandible but does not cause its expansion; and Type III: Cavity depth reaches the buccal cortex of the mandible and causes its expansion [11]. The present case was compatible with type II.
In the literature, four locations of SBC states have been provided: posterior lingual, anterior lingual, and buccal and lingual aspects of ascending ramus. Among these types, the most common one is the posterior lingual variant that can be seen on radiograph in submandibular gland fossa with an incidence of 0.10% to 0.48% [1, 9]. Anterior lingual type of SBC was first introduced by Richard and Ziskind in 1957. The anterior variant is seven times less frequent (incidence rate is even less than 0.009%)[1, 7, 10] and is usually located between the lower incisor and the premolar area above the insertion of mylohyoid muscle [6, 10, 12, 13]. The other types are extremely rare as an unusual finding [9].
The exact pathogenesis of SBC is still unknown, but there are some hypotheses regarding it. Stafne suggested that this defect is the result of abnormal bone deposition in the region formerly occupied by cartilage [2, 14, 15]. Fordyce believed SBC is an anatomical congenital defect caused by embryonic remnants of the submandibular gland trapped inside the body during mandibular ossification based on his finding of glandular tissue into this defect when he biopsied 2 cases [16]. Kay et al. suggested that the ethiology was related to an abnormal facial artery and that the vascular pressure along the inferior border of the mandible could lead to necrosis and bone resorption [17]. It is also said that the influence of arterial pulses can cause bone resorption as patients with hypertension tend to have SBC [18, 19].
Lello and Makek believed that these cavities resulted from focal bone atrophy due to an ischemic process associated with arterial degeneration change [20]. Philipsen et al. also declared that hyperplastic or hypertrophic salivary glands’ pressure on the bone surface can cause the formation of SBC [8]. However, the most commonly accepted view is that it originates from the pressure applied by glandular tissue on the lingual cortex of the mandible [7, 10, 21]. According to this opinion, the submandibular gland is related to the posterior variant of SBC, the sublingual gland is related to the anterior variant, and the parotid gland is related to the two variants of the ascending ramus of mandible [9]. However, Campos et al. showed that the mandibular ramus variant does not have such an origin because the parotid gland is not in contact with the lingual aspect of the ascending ramus of the mandible, which is covered by the medial pterygoid muscle [22]. The bone defect is either empty or frequently contains salivary gland, adipose tissue, connective tissue, muscles, blood vessels and rarely lymph nodes [4, 9, 14].
SBC can be readily differentiated from odontogenic lesions such as cysts because the epicenter of odontogenic lesions is located above the inferior alveolar canal. However, when the defect is related to the sublingual gland and appears above the canal, odontogenic lesions should be considered in the differential diagnosis [1]. SBCs in the posterior region of the mandible usually have typical radiograph features that make an easy diagnosis. However, this is not true for the anterior variant because they are usually noted between or below the teeth roots or are superimposed over the roots or at locations of the previous extraction site [23].
Most case reports of stafne bone cavities have discussed the findings on intraoral radiographs and the plain films of the mandible. Although these imaging techniques are often sufficient for diagnosis, they may not be definitive when the lesion is atypical such as lobulated, incompletely corticated, multiple or in an uncharacteristic location [6, 14, 24]. The three-dimensional images will assist in the final diagnosis of SBC. The size and extent of the cavity are best seen with CT imaging using both soft tissue and bone window settings [9]. CBCT is currently considered as the complementary modality of choice [3]. In his article, Venkatesh E. stated that CBCT was very helpful in analyzing and establishing a negative relationship with dentition and the mandibular canal and SBC; he also stated that this technique had limited area of exposure, which is an added advantage [25].
Segev et al. declared that the detection of SBC with CT is easier than with magnetic resonance imaging (MRI), but they also mentioned that MRI should be considered in order to identify the content of the cavity [7, 14, 26]. The main advantages of MRI are its superior soft tissue characterization and discrimination. The superior soft tissue contrast of MRI should be adequate to make the diagnosis of SBC, without any intravenous contrast material. However, the major disadvantages of MRI are its high cost and the distortion artifacts produced by dental material [14]. Sialography has been used to confirm the diagnosis by depicting salivary ducts within the bony defects [27], but there are case reports of surgically-proven stafne bone cavities with negative sialograms [28].
Sialography can be difficult to perform and uncomfortable for the patient, and it exposes the patient to ionizing radiation [24]. Nikzad et al. used CT densitometry by colorful differentiation in the diagnosis of SBC without the need for histopathology and could quickly individualize the content of defective area from the adjacent tissues [29]. Treatment is not recommended, but periodic follow-up along with panoramic radiograph is available, although the cavity is static and benign in nature [9, 30]. Surgical exploration, incisional biopsy, and enucleation are frequently done only for diagnostic reasons 13).
In the case of anterior, most of the time, endodontic treatment is undertaken due to misdiagnosed as inflammatory periapical lesions. Biopsy is usually undertaken following failure of endodontic treatment. Thus, to avoid unnecessary endodontic treatment for such lesions, vitality pulp test must be performed [31]. In the presented case, vitality test was performed and the canine tooth was found to be necrosis, but CBCT examination revealed that the lucency is not related to the tooth and is a bone defect.
3. Conclusion
Anterior variant of SBC is extremely rare. Advanced imaging modalities such as CBCT should be used for precise diagnosis.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declared no conflicts of interest.
Refrences
2. Discussion
Lingual mandibular bone depression represents a group of cavities in the lingual surface of the mandible while they have intact outer cortex. Historically, they were referred to as pseudocysts because they resemble a cyst in radiographic examination. It should be noted here that they are not true cysts because no epithelial lining is present in histology [1].
These defects were first introduced by Edward Stafne in 1942 [2]. He described these defects as asymptomatic and well-defined radiolucent cavities that were unilaterally located in the posterior region of the mandible between the mandibular angle and the third molar below the inferior dental canal. In his words, these defects were “bone cavities situated near the angle of the mandible” [3-8]. This asymptomatic defect is more likely to occur in men with a ratio of 6:1 and is usually observed at the age of over 40 years [5, 7, 9, 10].
These cavities are also known as lingual mandibular bone depression, developmental salivary gland defect, stafne defect, Stafne Bone Cyst (SBC), static bone cavity, latent bone cyst, and idiopathic bone cavity [1, 6].
Ariji et al. used CBCT to classify SBCs according to the depth of the cavity, as shown below: Type I: Cavity depth is limited to the medullar portion of the mandible; Type II: Cavity depth reaches the buccal cortex of the mandible but does not cause its expansion; and Type III: Cavity depth reaches the buccal cortex of the mandible and causes its expansion [11]. The present case was compatible with type II.
In the literature, four locations of SBC states have been provided: posterior lingual, anterior lingual, and buccal and lingual aspects of ascending ramus. Among these types, the most common one is the posterior lingual variant that can be seen on radiograph in submandibular gland fossa with an incidence of 0.10% to 0.48% [1, 9]. Anterior lingual type of SBC was first introduced by Richard and Ziskind in 1957. The anterior variant is seven times less frequent (incidence rate is even less than 0.009%)[1, 7, 10] and is usually located between the lower incisor and the premolar area above the insertion of mylohyoid muscle [6, 10, 12, 13]. The other types are extremely rare as an unusual finding [9].
The exact pathogenesis of SBC is still unknown, but there are some hypotheses regarding it. Stafne suggested that this defect is the result of abnormal bone deposition in the region formerly occupied by cartilage [2, 14, 15]. Fordyce believed SBC is an anatomical congenital defect caused by embryonic remnants of the submandibular gland trapped inside the body during mandibular ossification based on his finding of glandular tissue into this defect when he biopsied 2 cases [16]. Kay et al. suggested that the ethiology was related to an abnormal facial artery and that the vascular pressure along the inferior border of the mandible could lead to necrosis and bone resorption [17]. It is also said that the influence of arterial pulses can cause bone resorption as patients with hypertension tend to have SBC [18, 19].
Lello and Makek believed that these cavities resulted from focal bone atrophy due to an ischemic process associated with arterial degeneration change [20]. Philipsen et al. also declared that hyperplastic or hypertrophic salivary glands’ pressure on the bone surface can cause the formation of SBC [8]. However, the most commonly accepted view is that it originates from the pressure applied by glandular tissue on the lingual cortex of the mandible [7, 10, 21]. According to this opinion, the submandibular gland is related to the posterior variant of SBC, the sublingual gland is related to the anterior variant, and the parotid gland is related to the two variants of the ascending ramus of mandible [9]. However, Campos et al. showed that the mandibular ramus variant does not have such an origin because the parotid gland is not in contact with the lingual aspect of the ascending ramus of the mandible, which is covered by the medial pterygoid muscle [22]. The bone defect is either empty or frequently contains salivary gland, adipose tissue, connective tissue, muscles, blood vessels and rarely lymph nodes [4, 9, 14].
SBC can be readily differentiated from odontogenic lesions such as cysts because the epicenter of odontogenic lesions is located above the inferior alveolar canal. However, when the defect is related to the sublingual gland and appears above the canal, odontogenic lesions should be considered in the differential diagnosis [1]. SBCs in the posterior region of the mandible usually have typical radiograph features that make an easy diagnosis. However, this is not true for the anterior variant because they are usually noted between or below the teeth roots or are superimposed over the roots or at locations of the previous extraction site [23].
Most case reports of stafne bone cavities have discussed the findings on intraoral radiographs and the plain films of the mandible. Although these imaging techniques are often sufficient for diagnosis, they may not be definitive when the lesion is atypical such as lobulated, incompletely corticated, multiple or in an uncharacteristic location [6, 14, 24]. The three-dimensional images will assist in the final diagnosis of SBC. The size and extent of the cavity are best seen with CT imaging using both soft tissue and bone window settings [9]. CBCT is currently considered as the complementary modality of choice [3]. In his article, Venkatesh E. stated that CBCT was very helpful in analyzing and establishing a negative relationship with dentition and the mandibular canal and SBC; he also stated that this technique had limited area of exposure, which is an added advantage [25].
Segev et al. declared that the detection of SBC with CT is easier than with magnetic resonance imaging (MRI), but they also mentioned that MRI should be considered in order to identify the content of the cavity [7, 14, 26]. The main advantages of MRI are its superior soft tissue characterization and discrimination. The superior soft tissue contrast of MRI should be adequate to make the diagnosis of SBC, without any intravenous contrast material. However, the major disadvantages of MRI are its high cost and the distortion artifacts produced by dental material [14]. Sialography has been used to confirm the diagnosis by depicting salivary ducts within the bony defects [27], but there are case reports of surgically-proven stafne bone cavities with negative sialograms [28].
Sialography can be difficult to perform and uncomfortable for the patient, and it exposes the patient to ionizing radiation [24]. Nikzad et al. used CT densitometry by colorful differentiation in the diagnosis of SBC without the need for histopathology and could quickly individualize the content of defective area from the adjacent tissues [29]. Treatment is not recommended, but periodic follow-up along with panoramic radiograph is available, although the cavity is static and benign in nature [9, 30]. Surgical exploration, incisional biopsy, and enucleation are frequently done only for diagnostic reasons 13).
In the case of anterior, most of the time, endodontic treatment is undertaken due to misdiagnosed as inflammatory periapical lesions. Biopsy is usually undertaken following failure of endodontic treatment. Thus, to avoid unnecessary endodontic treatment for such lesions, vitality pulp test must be performed [31]. In the presented case, vitality test was performed and the canine tooth was found to be necrosis, but CBCT examination revealed that the lucency is not related to the tooth and is a bone defect.
3. Conclusion
Anterior variant of SBC is extremely rare. Advanced imaging modalities such as CBCT should be used for precise diagnosis.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declared no conflicts of interest.
Refrences
- White SC, Pharoah MJ. Principles and interpretation of Oral Radiology.( 7th Ed). Amsterdam: Elsevier; 2014.
- Stafne EC. Bone cavities situated near the angle of the mandible. The Journal of the American Dental Association. 1942; 29(17):1969-72. doi: 10.14219/jada.archive.1942.0315
- Münevveroğlu AP, Aydın KC. Stafne bone defect: report of two cases. Case reports in Dentistry. 2012; 2012:1–5. doi: 10.1155/2012/654839
- Monteiro LS, Da Câmara MI, Tadeu F, Salazar F, Pacheco JJ. Posterior lingual bone depression diagnosis using 3D-computed tomography. Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial. 2012; 53(3):170-4. doi: 10.1016/j.rpemd.2012.05.007
- Etöz M, Etöz OA, Şahman H, Şekerci AE, Polat HB. An unusual case of multilocular Stafne bone cavity. Dentomaxillofacial Radiology. 2012; 41(1):75-8. doi: 10.1259/dmfr/34731967
- Sisman Y, Etöz OA, Mavili E, Sahman H, Tarim Ertas E. Anterior Stafne bone defect mimicking a residual cyst: A case report. Dentomaxillofacial Radiology. 2010; 39(2):124-6. doi: 10.1259/dmfr/49320253
- Dolanmaz D, Etöz OA, Pampu AA, Kılıç E, Şişman Y. Diagnosis of Stafne’s bone cavity with dental computerized tomography. European Journal of General Medicine. 2009; 6(1):42–5. doi: 10.29333/ejgm/82635
- Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y. Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofacial Radiology. 2002; 31(5):281-90. doi: 10.1038/sj.dmfr.4600718
- More CB, Das S, Gupta S, Patel P, Saha N. Stafne’s bone cavity: A diagnostic challenge. Journal of Clinical and Diagnostic Research. 2015; 9(11):ZD16–ZD19. PMCID: PMC4668534
- Sisman Y, Miloglu O, Sekerci AE, Yilmaz AB, Demirtas O, Tokmak TT. Radiographic evaluation on prevalence of Stafne bone defect: a study from two centres in Turkey. Dentomaxillofacial Radiology. 2012; 41(2):152-8. doi: 10.1259/dmfr/10586700
- Ariji E, Fujiwara N, Tabata O, Nakayama E, Kanda S, Shiratsuchi Y, Oka M. Stafne's bone cavity: Classification based on outline and content determined by computed tomography. Oral Surgery, Oral Medicine, Oral Pathology. 1993; 76(3):375-80. doi: 10.1016/0030-4220(93)90271-5
- Richard EL, Ziskind J. Aberrant salivary gland tissue in mandible. Oral Surgery, Oral Medicine, Oral Pathology. 1957; 10(10):1086-90. doi: 10.1016/0030-4220(57)90059-2
- Khalesi S, Deyhimi P, Darisavi S. Stafne bone cavity with ectopic salivary gland tissue in the anterior of mandible. Dental research journal. 2016; 13(5):454. doi: 10.4103/1735-3327.192306
- Segev Y, Puterman M, Bodner L. Stafne bone cavity: magnetic resonance imaging. Medicina Oral, Patología Oral y Cirugía Bucal. 2006; 11(4):E345-7. PMID: 16816811
- Aguiar LB, Neves FS, Bastos LC, Crusoé-Rebello I, Ambrosano GM, Campos PS. Multiple Stafne bone defects: A rare entity. ISRN Dentistry. 2011; 2011:1–3. doi: /10.5402/2011/792145
- Fordyce GL. The probable nature of so-called latent haemorrhagic cysts of the mandible. British Dental Journal. 1956; 101(1):40-2.
- Kay LW. Some anthropologic investigations of interest to oral surgeons. International Journal of Oral Surgery. 1974; 3(6):363-79. doi: 10.1016/s0300-9785(74)80001-3
- Shimizu M, Osa N, Okamura K, Yoshiura K. CT analysis of the Stafne's bone defects of the mandible. Dentomaxillofacial Radiology. 2006; 35(2):95-102. doi: 10.1259/dmfr/71115878
- Minowa K, Inoue N, Sawamura T, Matsuda A, Totsuka Y, Nakamura M. Evaluation of static bone cavities with CT and MRI. Dentomaxillofacial Radiology. 2003; 32(1):2-7. doi: 10.1259/dmfr/92201340
- Lello GE, Makek M. Stafne's mandibularlingual cortical defect discussion of aetiology. Journal of Maxillofacial Surgery. 1985; 13:172-6. doi: 10.1016/s0301-0503(85)80042-4
- Belmonte-Caro R, Velez-Gutierrez MJ, García DL, García-Perla-García A, Infante-Cossío PA, Díaz-Fernández JM, et al. A Stafne's cavity with unusual location in the mandibular anterior area. Medicina Oral, Patologia Oral y Cirugia Bucal. 2005; 10(2):173-9. PMID: 15735551
- Campos PS, Panella J, Crusoé-Rebello IM, Azevedo RA, Pena N, Cunha T. Mandibular ramus-related Stafne's bone cavity. Dentomaxillofacial Radiology. 2004; 33(1):63-6. doi: 10.1259/dmfr/39682286
- De Courten A, Küffer R, Samson J, Lombardi T. Anterior lingual mandibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2002; 94(4):460-4. doi: 10.1067/moe.2002.125196
- Branstetter BF, Weissman JL, Kaplan SB. Imaging of a Stafne bone cavity: What MR adds and why a new name is needed. American Journal of Neuroradiology. 1999; 20(4):587-9. PMID: 10319966
- Venkatesh E. Stafne bone cavity and cone-beam computed tomography: A report of two cases. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2015 ; 41(3):145-8. doi: 10.5125/jkaoms.2015.41.3.145
- Ertas ET, Atici MY, Kalabalik F, Ince O. Investigation and differential diagnosis of Stafne bone cavities with cone beam computed tomography and magnetic resonance imaging: Report of two cases. Journal of Oral and Maxillofacial Radiology. 2015; 3(3):92. doi: 10.4103/2321-3841.170617
- Tominaga K, Kuga Y, Kubota K, Ohba T. Stafne's bone cavity in the anterior mandible: Report of a case. Dentomaxillofacial Radiology. 1990; 19(1):28-30. doi: 10.1259/dmfr.19.1.2387472
- Oikarinen VJ, Wolf J, Julku M. A stereosialographic study of developmental mandibular bone defects (Stafne's idiopathic bone cavities). International Journal of Oral Surgery. 1975; 4(2):51-4. doi: 10.1016/s0300-9785(75)80012-3
- Nikzad S, Azari AB, Khezri FH. Diagnosis of a Lingual Mandibular Bone Defect (Stafne's Bone Defect) by CT Scan. Iranian Journal of Radiology. 2010; 7(1):27-30.
- Anbiaee N, Ebrahimi S, Ebrahimnejad H, Mohammadzade Rezaie M, Sahebnasagh Z, et al. Stafne bone defect in the ramus of the mandible: A case report. Journal of Dentomaxillofacial Radiology, Pathology and Surgery. 2016; 5(1):37–41. doi: 10.18869/acadpub.3dj.5.1.37
- Turkoglu K, Orhan K. Stafne bone cavity in the anterior mandible. Journal of Craniofacial Surgery. 2010; 21(6):1769-75. doi: 10.1097/scs.0b013e3181f40347
Type of Study: Original article |
Subject:
So on
Received: 2017/04/22 | Accepted: 2017/06/10 | Published: 2017/10/1
Received: 2017/04/22 | Accepted: 2017/06/10 | Published: 2017/10/1
References
1. White SC, Pharoah MJ. Principles and interpretation of Oral Radiology. (7th Ed). Amsterdam: Elsevier; 2014.
2. Stafne EC. Bone cavities situated near the angle of the mandible. The Journal of the American Dental Association. 1942; 29(17):1969-72. doi: 10.14219/jada.archive.1942.0315 [DOI:10.14219/jada.archive.1942.0315]
3. Münevveroğlu AP, Aydın KC. Stafne bone defect: report of two cases. Case reports in Dentistry. 2012; 2012:1–5. doi: 10.1155/2012/654839 [DOI:10.1155/2012/654839]
4. Monteiro LS, Da Câmara MI, Tadeu F, Salazar F, Pacheco JJ. Posterior lingual bone depression diagnosis using 3D-computed tomography. Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial. 2012; 53(3):170-4. doi: 10.1016/j.rpemd.2012.05.007 [DOI:10.1016/j.rpemd.2012.05.007]
5. Etöz M, Etöz OA, Şahman H, Şekerci AE, Polat HB. An unusual case of multilocular Stafne bone cavity. Dentomaxillofacial Radiology. 2012; 41(1):75-8. doi: 10.1259/dmfr/34731967 [DOI:10.1259/dmfr/34731967]
6. Sisman Y, Etöz OA, Mavili E, Sahman H, Tarim Ertas E. Anterior Stafne bone defect mimicking a residual cyst: A case report. Dentomaxillofacial Radiology. 2010; 39(2):124-6. doi: 10.1259/dmfr/49320253 [DOI:10.1259/dmfr/49320253]
7. Dolanmaz D, Etöz OA, Pampu AA, Kılıç E, Şişman Y. Diagnosis of Stafne's bone cavity with dental computerized tomography. European Journal of General Medicine. 2009; 6(1):42–5. doi: 10.29333/ejgm/82635 [DOI:10.29333/ejgm/82635]
8. Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y. Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofacial Radiology. 2002; 31(5):281-90. doi: 10.1038/sj.dmfr.4600718 [DOI:10.1038/sj.dmfr.4600718]
9. More CB, Das S, Gupta S, Patel P, Saha N. Stafne's bone cavity: A diagnostic challenge. Journal of Clinical and Diagnostic Research. 2015; 9(11):ZD16–ZD19. PMCID: PMC4668534 [DOI:10.7860/JCDR/2015/14273.6772]
10. Sisman Y, Miloglu O, Sekerci AE, Yilmaz AB, Demirtas O, Tokmak TT. Radiographic evaluation on prevalence of Stafne bone defect: a study from two centres in Turkey. Dentomaxillofacial Radiology. 2012; 41(2):152-8. doi: 10.1259/dmfr/10586700 [DOI:10.1259/dmfr/10586700]
11. Ariji E, Fujiwara N, Tabata O, Nakayama E, Kanda S, Shiratsuchi Y, Oka M. Stafne's bone cavity: Classification based on outline and content determined by computed tomography. Oral Surgery, Oral Medicine, Oral Pathology. 1993; 76(3):375-80. doi: 10.1016/0030-4220(93)90271-5 [DOI:10.1016/0030-4220(93)90271-5]
12. Richard EL, Ziskind J. Aberrant salivary gland tissue in mandible. Oral Surgery, Oral Medicine, Oral Pathology. 1957; 10(10):1086-90. doi: 10.1016/0030-4220(57)90059-2 [DOI:10.1016/0030-4220(57)90059-2]
13. Khalesi S, Deyhimi P, Darisavi S. Stafne bone cavity with ectopic salivary gland tissue in the anterior of mandible. Dental research journal. 2016; 13(5):454. doi: 10.4103/1735-3327.192306 [DOI:10.4103/1735-3327.192306]
14. Segev Y, Puterman M, Bodner L. Stafne bone cavity: magnetic resonance imaging. Medicina Oral, Patología Oral y Cirugía Bucal. 2006; 11(4):E345-7. PMID: 16816811 [PMID]
15. Aguiar LB, Neves FS, Bastos LC, Crusoé-Rebello I, Ambrosano GM, Campos PS. Multiple Stafne bone defects: A rare entity. ISRN Dentistry. 2011; 2011:1–3. doi: /10.5402/2011/792145
16. Fordyce GL. The probable nature of so-called latent haemorrhagic cysts of the mandible. British Dental Journal. 1956; 101(1):40-2.
17. Kay LW. Some anthropologic investigations of interest to oral surgeons. International Journal of Oral Surgery. 1974; 3(6):363-79. doi: 10.1016/s0300-9785(74)80001-3 [DOI:10.1016/S0300-9785(74)80001-3]
18. Shimizu M, Osa N, Okamura K, Yoshiura K. CT analysis of the Stafne's bone defects of the mandible. Dentomaxillofacial Radiology. 2006; 35(2):95-102. doi: 10.1259/dmfr/71115878 [DOI:10.1259/dmfr/71115878]
19. Minowa K, Inoue N, Sawamura T, Matsuda A, Totsuka Y, Nakamura M. Evaluation of static bone cavities with CT and MRI. Dentomaxillofacial Radiology. 2003; 32(1):2-7. doi: 10.1259/dmfr/92201340 [DOI:10.1259/dmfr/92201340]
20. Lello GE, Makek M. Stafne's mandibularlingual cortical defect discussion of aetiology. Journal of Maxillofacial Surgery. 1985; 13:172-6. doi: 10.1016/s0301-0503(85)80042-4 [DOI:10.1016/S0301-0503(85)80042-4]
21. Belmonte-Caro R, Velez-Gutierrez MJ, García DL, García-Perla-García A, Infante-Cossío PA, Díaz-Fernández JM, et al. A Stafne's cavity with unusual location in the mandibular anterior area. Medicina Oral, Patologia Oral y Cirugia Bucal. 2005; 10(2):173-9. PMID: 15735551 [PMID]
22. Campos PS, Panella J, Crusoé-Rebello IM, Azevedo RA, Pena N, Cunha T. Mandibular ramus-related Stafne's bone cavity. Dentomaxillofacial Radiology. 2004; 33(1):63-6. doi: 10.1259/dmfr/39682286 [DOI:10.1259/dmfr/39682286]
23. De Courten A, Küffer R, Samson J, Lombardi T. Anterior lingual mandibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2002; 94(4):460-4. doi: 10.1067/moe.2002.125196 [DOI:10.1067/moe.2002.125196]
24. Branstetter BF, Weissman JL, Kaplan SB. Imaging of a Stafne bone cavity: What MR adds and why a new name is needed. American Journal of Neuroradiology. 1999; 20(4):587-9. PMID: 10319966 [PMID]
25. Venkatesh E. Stafne bone cavity and cone-beam computed tomography: A report of two cases. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2015 ; 41(3):145-8. doi: 10.5125/jkaoms.2015.41.3.145 [DOI:10.5125/jkaoms.2015.41.3.145]
26. Ertas ET, Atici MY, Kalabalik F, Ince O. Investigation and differential diagnosis of Stafne bone cavities with cone beam computed tomography and magnetic resonance imaging: Report of two cases. Journal of Oral and Maxillofacial Radiology. 2015; 3(3):92. doi: 10.4103/2321-3841.170617 [DOI:10.4103/2321-3841.170617]
27. Tominaga K, Kuga Y, Kubota K, Ohba T. Stafne's bone cavity in the anterior mandible: Report of a case. Dentomaxillofacial Radiology. 1990; 19(1):28-30. doi: 10.1259/dmfr.19.1.2387472 [DOI:10.1259/dmfr.19.1.2387472]
28. Oikarinen VJ, Wolf J, Julku M. A stereosialographic study of developmental mandibular bone defects (Stafne's idiopathic bone cavities). International Journal of Oral Surgery. 1975; 4(2):51-4. doi: 10.1016/s0300-9785(75)80012-3 [DOI:10.1016/S0300-9785(75)80012-3]
29. Nikzad S, Azari AB, Khezri FH. Diagnosis of a Lingual Mandibular Bone Defect (Stafne's Bone Defect) by CT Scan. Iranian Journal of Radiology. 2010; 7(1):27-30.
30. Anbiaee N, Ebrahimi S, Ebrahimnejad H, Mohammadzade Rezaie M, Sahebnasagh Z, et al. Stafne bone defect in the ramus of the mandible: A case report. Journal of Dentomaxillofacial Radiology, Pathology and Surgery. 2016; 5(1):37–41. doi: 10.18869/acadpub.3dj.5.1.37 [DOI:10.18869/acadpub.3dj.5.1.37]
31. Turkoglu K, Orhan K. Stafne bone cavity in the anterior mandible. Journal of Craniofacial Surgery. 2010; 21(6):1769-75. doi: 10.1097/scs.0b013e3181f40347 [DOI:10.1097/SCS.0b013e3181f40347]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |