Thu, Jan 29, 2026
Volume 14, Issue 3 (9-2025)
2025, 14(3): 24-32 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Chokami H S, Ostovarrad F, Javidi P, Tabari Khomeiran R, Rostami A. Prevalence of Soft Palate Morphologies in Patients with Cleft Palate: A Cross-sectional Study (2017–2019). Journal title 2025; 14 (3) :24-32
URL: http://3dj.gums.ac.ir/article-1-653-en.html
URL: http://3dj.gums.ac.ir/article-1-653-en.html
Hamidreza Sharifipour Chokami1 

 , Farzaneh Ostovarrad2
, Farzaneh Ostovarrad2 

 , Pedram Javidi3
, Pedram Javidi3 

 , Rasoul Tabari Khomeiran4
, Rasoul Tabari Khomeiran4 

 , Amirreza Rostami *5
, Amirreza Rostami *5 




 , Farzaneh Ostovarrad2
, Farzaneh Ostovarrad2 

 , Pedram Javidi3
, Pedram Javidi3 

 , Rasoul Tabari Khomeiran4
, Rasoul Tabari Khomeiran4 

 , Amirreza Rostami *5
, Amirreza Rostami *5 


1- School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Orthodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. ,Arezarostami74@gmail.com
2- Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Orthodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Medical Surgical Nursing, School of Nursing and Midwifery, Guilan University of Medical Sciences, Rasht, Iran.
5- Department of Oral and Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. ,
Keywords: Cleft Palate, Radiography Velopharyngeal Sphincter
Full-Text [PDF 997 kb]
(175 Downloads)
| Abstract (HTML) (235 Views)
Full-Text: (2 Views)
1. Introduction
Facial development initiates during the fourth week of embryogenesis with the emergence of medial nasal prominences, lateral nasal prominences, and maxillary prominences. Cleft lip arises from incomplete fusion of the medial nasal prominences (either with each other or the maxillary prominences), whereas cleft palate results from failed fusion of the palatal shelves (typically between weeks 8–12 of gestation) (1, 2).
The soft palate, a posterior fibromuscular extension of the palate connected to the posterior margin of the hard palate, comprises the levator veli palatini, tensor veli palatini, palatoglossus, palatopharyngeus, and musculus uvulae. It plays a vital role in swallowing, breathing, and speech (3). Dysfunction of the soft palate can result from various factors, including cleft lip and palate, enlarged adenoids, obstructive sleep apnea syndrome (OSAS), snoring, poorly maintained maxillary dentures, and craniofacial skeletal malocclusions. Understanding the normal anatomy and morphological variations of the soft palate is crucial for diagnosing and effectively managing these conditions (4, 5).
Cleft palate, a congenital disorder influenced by geographic, racial, and socioeconomic factors, has a global prevalence of 1 in 500–2,500 live births. More specific epidemiological data indicate that orofacial clefts overall, including cleft palate, occur in about 1 in 1,000 to 1,500 live births globally, which aligns with the general prevalence estimates often cited (6, 7). Patients often experience swallowing difficulties, speech impairments, and aesthetic concerns, necessitating surgical and prosthetic interventions to improve function and psychosocial well-being (8, 9).
Velopharyngeal dysfunction (VPD) is a primary speech complication in cleft palate patients. Insufficient soft palate mobility impairs its seal with the posterior pharyngeal wall, causing hypernasality and articulation disorders (10). It refers to the impaired function of the movable structures responsible for controlling the velopharyngeal sphincter. Approximately 30 % of patients who undergo cleft palate repair surgery require secondary surgical intervention due to persistent VPD. Understanding the normal anatomy and physiology of the velopharyngeal mechanism is the essential first step for an accurate diagnosis and effective treatment of children born with cleft lip and palate. The primary function of the velopharyngeal mechanism is to create a tight seal between the soft palate and the pharyngeal walls, thereby separating the oral and nasal cavities for various functions, including speech.
Velopharyngeal closure is accomplished through the coordinated contraction of several muscles, including the levator veli palatini, musculus uvulae, superior pharyngeal constrictor, palatopharyngeus, palatoglossus, and salpingopharyngeus (11, 12).
The primary goal of palatoplasty is to restore natural anatomy. Theoretically, palatoplasty improves the functional dynamics of the soft palate and pharyngeal walls by correcting dysmorphology in both the levator veli palatini and palatopharyngeus muscles (13). Pre- and postoperative anatomical assessments, along with short- and long-term outcome evaluations, enhance understanding of how different palatoplasty techniques influence soft palate structure. This is critical for optimizing velopharyngeal function, which underpins normal speech (14).
The Need’s ratio (soft palate length/pharyngeal depth) serves as a diagnostic tool for assessing velopharyngeal function. In individuals with normal anatomy, this ratio ranges between 0.6 and 0.7. Among the six soft palate morphologies classified by the You et al. classification system, type 6 (hook-shaped) demonstrates the highest soft-palate-to-pharyngeal-depth ratio (15, 16). Considering this issue, examining the type of soft palate morphology in patients with cleft palate can help in the early diagnosis and prevention of surgery caused by VPD. Deepa et al. (17) demonstrated morphological variations of the soft palate in the Indian population and identified multiple shapes such as rat-tail, butt-shape, and leaf-shape, with Rat-tail being the most common. It highlights no significant gender differences in soft palate types but notes variations in velar length with age and sex. Some shapes, like hook-shaped, may increase the risk of velopharyngeal insufficiency or sleep apnea.
Lateral cephalometric radiography is one of the most common extraoral radiographs after panoramic imaging, and it is applied in surgery and orthodontics treatment planning. It is used to measure anatomical distances and classify patients based on craniofacial morphology. As a standard diagnostic tool, it supports craniofacial assessment, treatment planning, progress monitoring, and outcome evaluation (18, 19). However, this technique projects three-dimensional craniofacial structures onto two-dimensional images, complicating accurate measurements even with optimal patient positioning (20). The main advantage of this technique is that the images obtained can be compared across different times and locations, allowing for the monitoring of growth, development, and treatment progress (21).
The soft palate has different morphologies in various diseases. Therefore, determining the different normal shapes of the soft palate in patients helps in the diagnosis and successful treatment of many complex cases and different diseases (22). There is a significant knowledge gap regarding the detailed morphological characteristics of the soft palate in cleft palate patients within the regional population, as no prior studies have specifically examined soft palate morphology among cleft palate patients in Guilan or similar regional settings. This lack of localized morphological data limits the understanding needed for tailored diagnosis and treatment planning in this population. Therefore, this study aimed to determine the frequency of soft palate morphology types in individuals with cleft palate among patients attending the dental schools of Guilan University of Medical Sciences from 2017-2019 using accessible lateral cephalometric radiographs.
2. Materials and Methods
This retrospective cross-sectional descriptive study was conducted on lateral cephalometric radiographs of 90 patients with isolated cleft palate who presented to the dental school at Guilan University of Medical Sciences from 2017 to 2019. The patients had cleft palate based on radiographic images. Automatic exposure settings with 60-90 kVp were used by the device to optimize the exposure conditions for each patient.
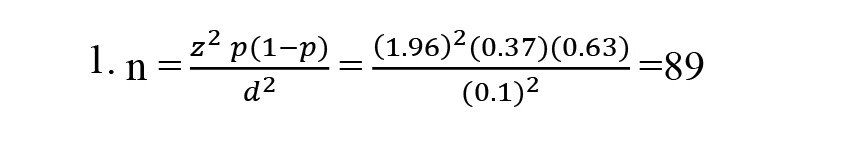
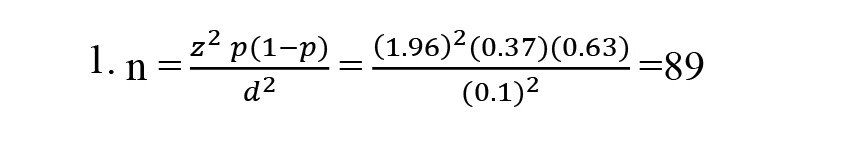
The required sample size was calculated to be n=89 based on a single proportion formula (Equation 1), assuming a 95% confidence level, 80% power, and an anticipated prevalence of 50% with a precision of 10%. To compensate for possible dropouts and missing data, the sample size was increased to 90 participants (23).
The sampling method of the study can be formally described as a systematic sampling approach with a reverse chronological order of selection. Specifically, lateral cephalometric radiographs of patients with cleft palate who met the inclusion criteria were systematically reviewed starting from the most recent radiographs and moving backward to older radiographs until the predetermined sample size of 89 was reached. This method ensured up-to-date data while maintaining a representative sample within the defined study period from 2017 to 2019. Only one radiograph per patient was included, duplicates were excluded, and radiographs with suboptimal quality or prior surgical intervention were omitted to enhance data validity. The rationale for reverse chronological selection is typically to capture the most current clinical presentations and imaging quality while avoiding selection bias inherent to arbitrary sampling. Observers were blinded to demographic details (age and sex) to reduce classification bias.
All lateral cephalograms were obtained using a Soredex Cranex (Helsinki, Finland) with cephalostat under standardized conditions. The patient’s head must be properly positioned with no rotation or tilt, maintaining the midsagittal plane perpendicular to the floor to avoid cephalometric distortion. The image must demonstrate clear visualization of critical anatomical landmarks with sharp contrast and no motion artifacts. Proper occlusion of the teeth is essential to allow accurate skeletal and dental analysis. Images must be free from external artifacts or obstructions that could interfere with interpretation. In the present study, any radiographs showing positioning inaccuracies such as head rotation beyond acceptable limits, poor image clarity, or suboptimal exposure conditions were excluded from analysis to maintain data quality. Manual analysis was performed using a negatoscope by one maxillofacial radiologist and one orthodontist, using tracing paper. The study employed the You et al. classification system (15) for soft palate morphology, comprising six types: The leaf-shaped form, in which the mid-portion is elevated toward the oral or nasal cavities; the rat-tail shaped type, characterized by anterior swelling with a distinct narrowing at the free edge; the butt-shaped form, which is short and wide with relatively uniform thickness; the straight-line type, showing a flat and planar configuration; the s-shaped (distorted soft palate), which presents an abnormal curvature resembling the letter “S”; and finally the hook-shaped form, where the posterior segment is curved anterosuperiorly, resembling a hook.
In cases where the morphology of the soft palate was ambiguous or borderline, these instances were managed through a consensus decision process between the two observers—a maxillofacial radiologist and an orthodontist—who independently analyzed the lateral cephalometric radiographs. When disagreement occurred on classification using the You et al. system (15), the observers reviewed the cases jointly to discuss the features and reach a mutual agreement. This approach ensured the reliability and accuracy of morphological classification by minimizing subjective bias and improving diagnostic consistency in borderline cases.
The inter-rater and intra-rater reliability for soft palate morphology classification were assessed using Cohen’s kappa coefficient, with values indicating excellent agreement. Cohen’s kappa was calculated by comparing the observed agreement between raters to the expected agreement by chance, expressed with a 95% confidence interval (CI). Values above 0.80 were interpreted as near-perfect agreement. Any classification disagreements were resolved through consensus discussions and joint image review to ensure consistent and reliable interpretation. This rigorous reliability assessment supports the robustness of the morphological data reported in this study. The descriptive analyses employed mean, frequency percentage, standard deviation, minimum, and maximum values. Statistical analysis was performed using Fisher’s exact test. Data processing was executed via SPSS software, version 19 and statistical significance was considered at 0.05.
3. Results
Based on the obtained results from Table 1, the number of participants in the study was equal in terms of gender. Moreover, the highest frequency is observed in the 15–20-year age group, comprising 32 individuals (35.6%), while the lowest frequency is found in the 30–35-year age group, with 16 individuals (17.7%).
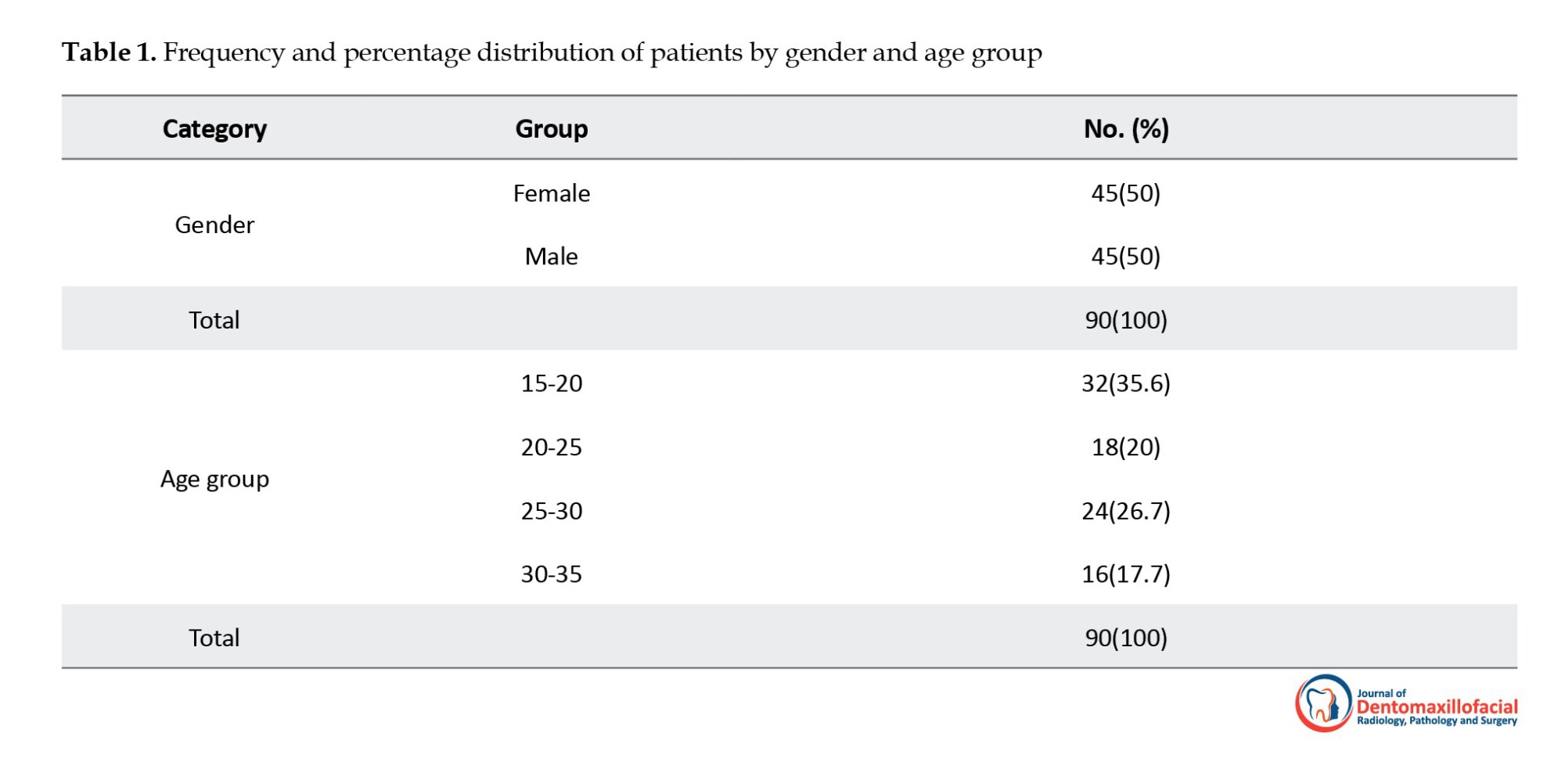
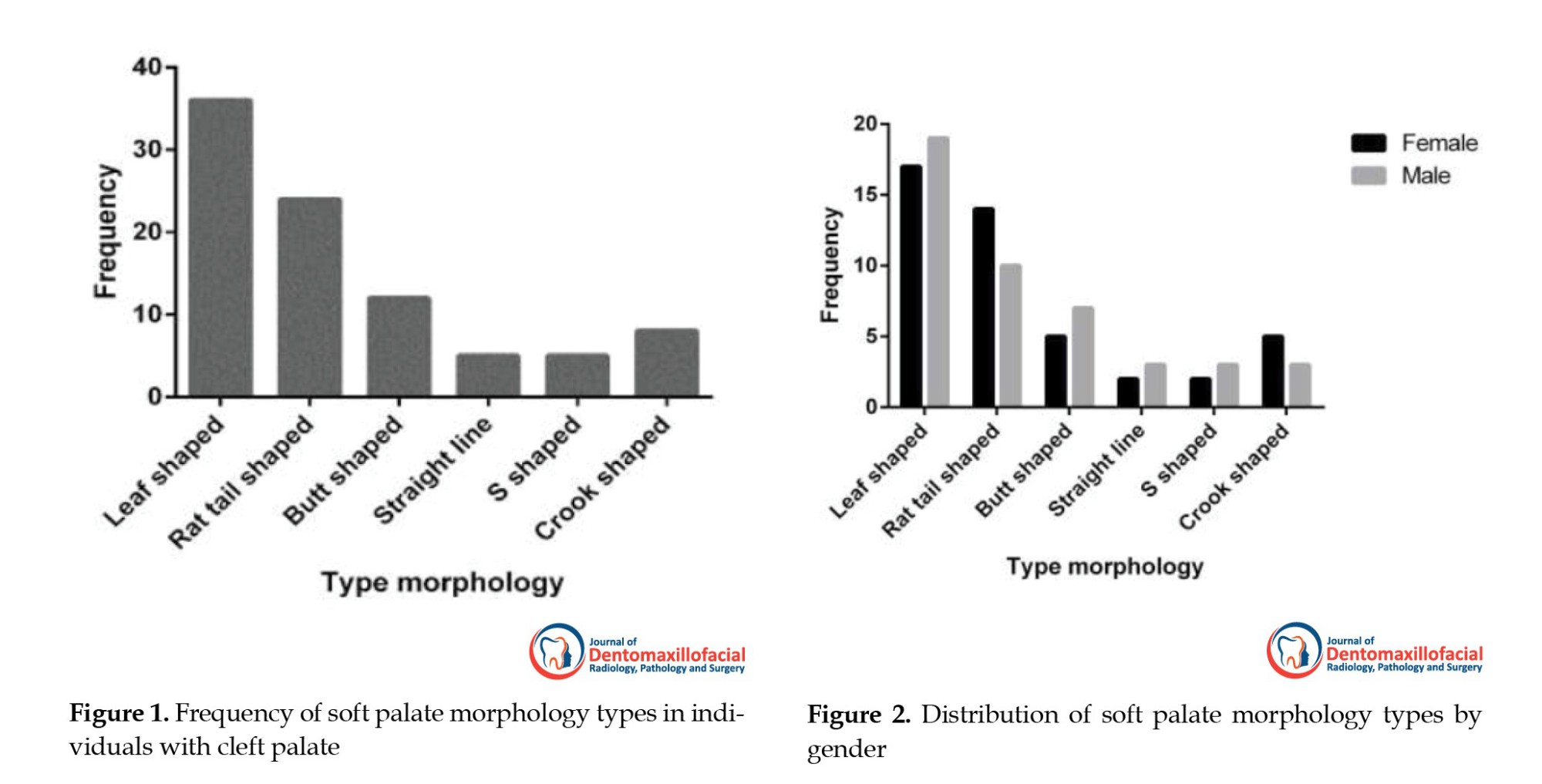
Figure 1 represents the frequency distribution of different soft palate morphology types, based on You et al. (15) classification system among individuals with cleft palate who attended dental schools at Guilan University of Medical Sciences. The results indicate that the leaf-shaped type had the highest frequency, with 36 cases (40%), while the straight-line and s-shaped had the lowest frequency, with 5 cases (5.6%). Figure 2 illustrates the distribution of morphology types by gender, showing similar patterns in males and females, with no remarkable differences.
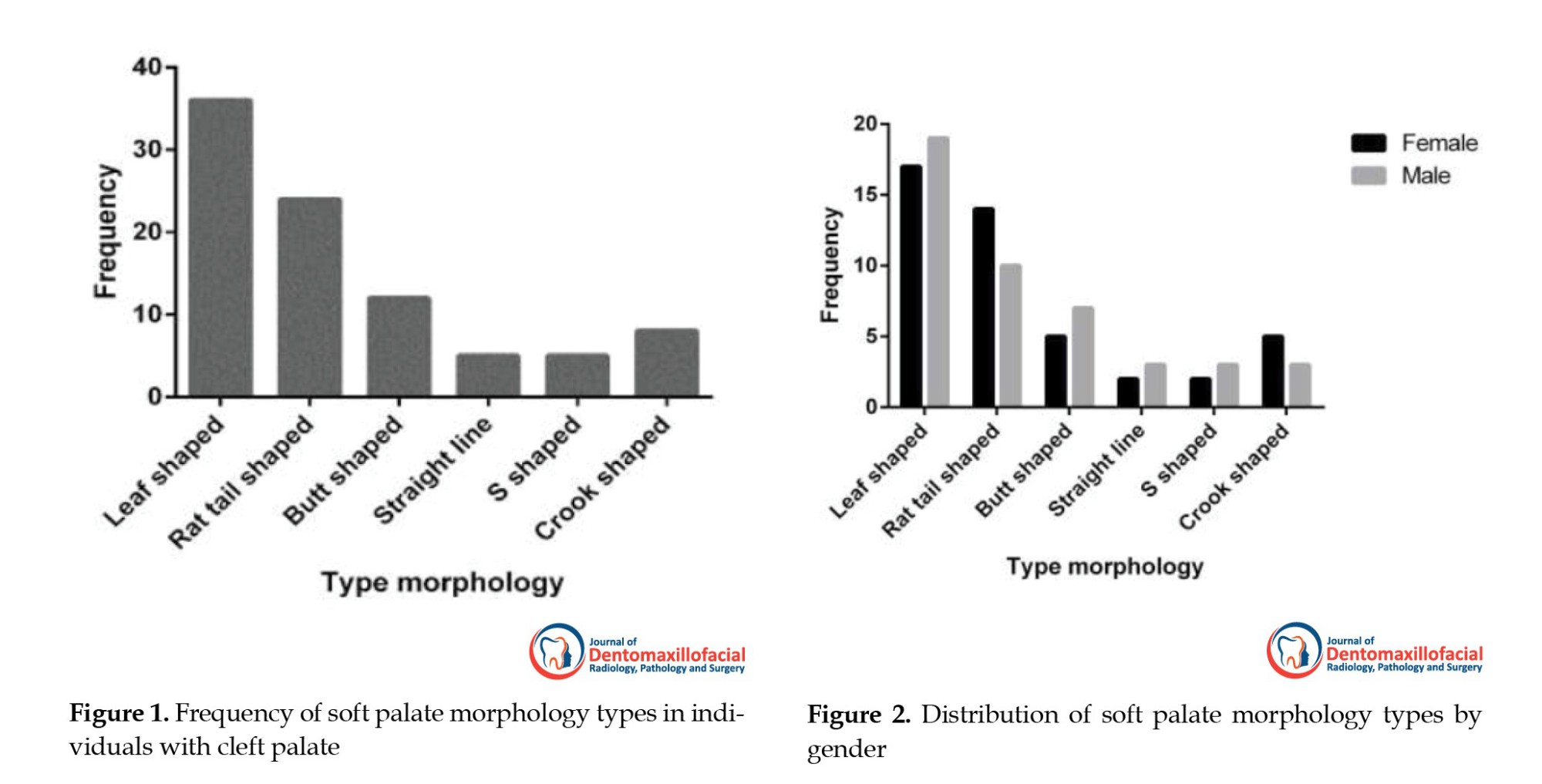
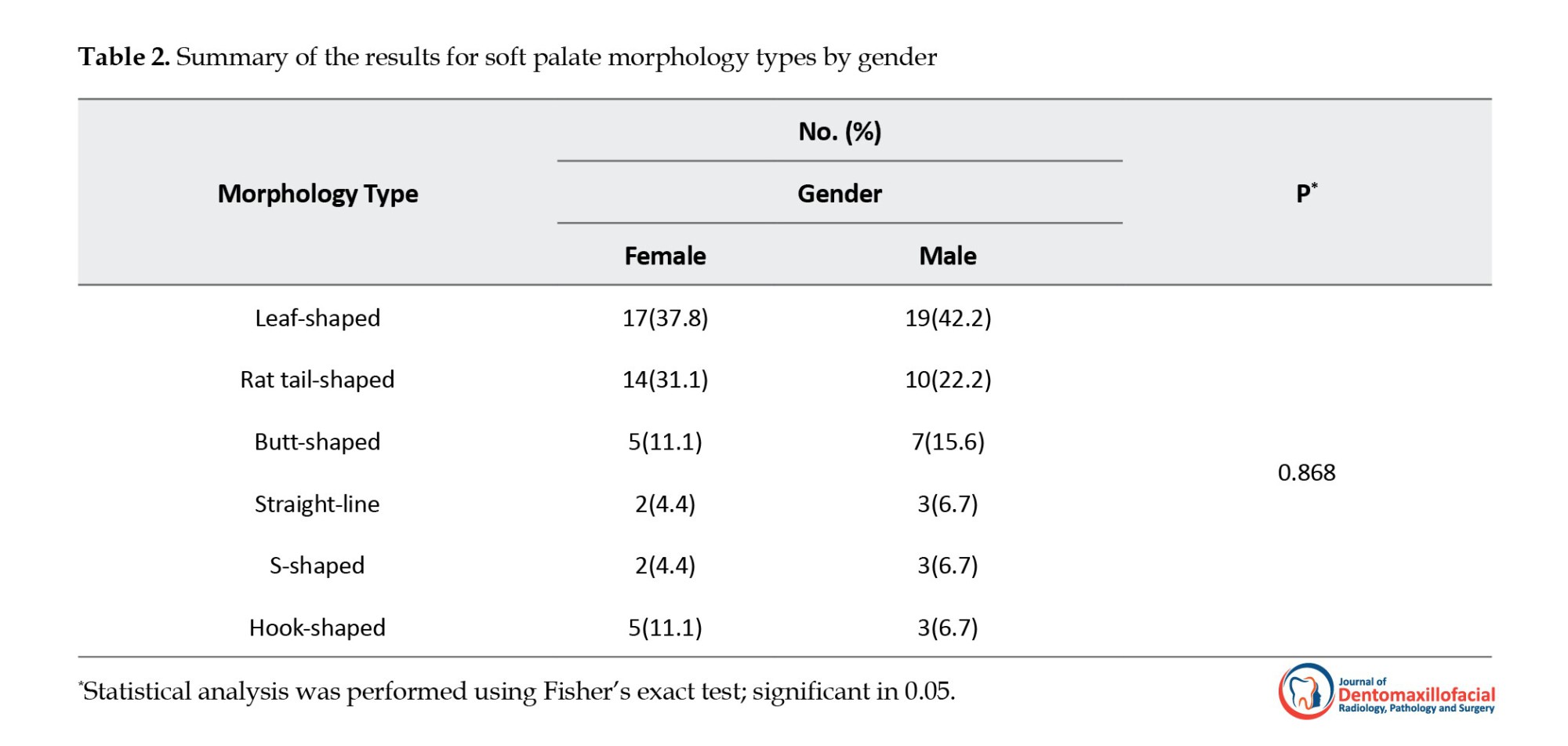
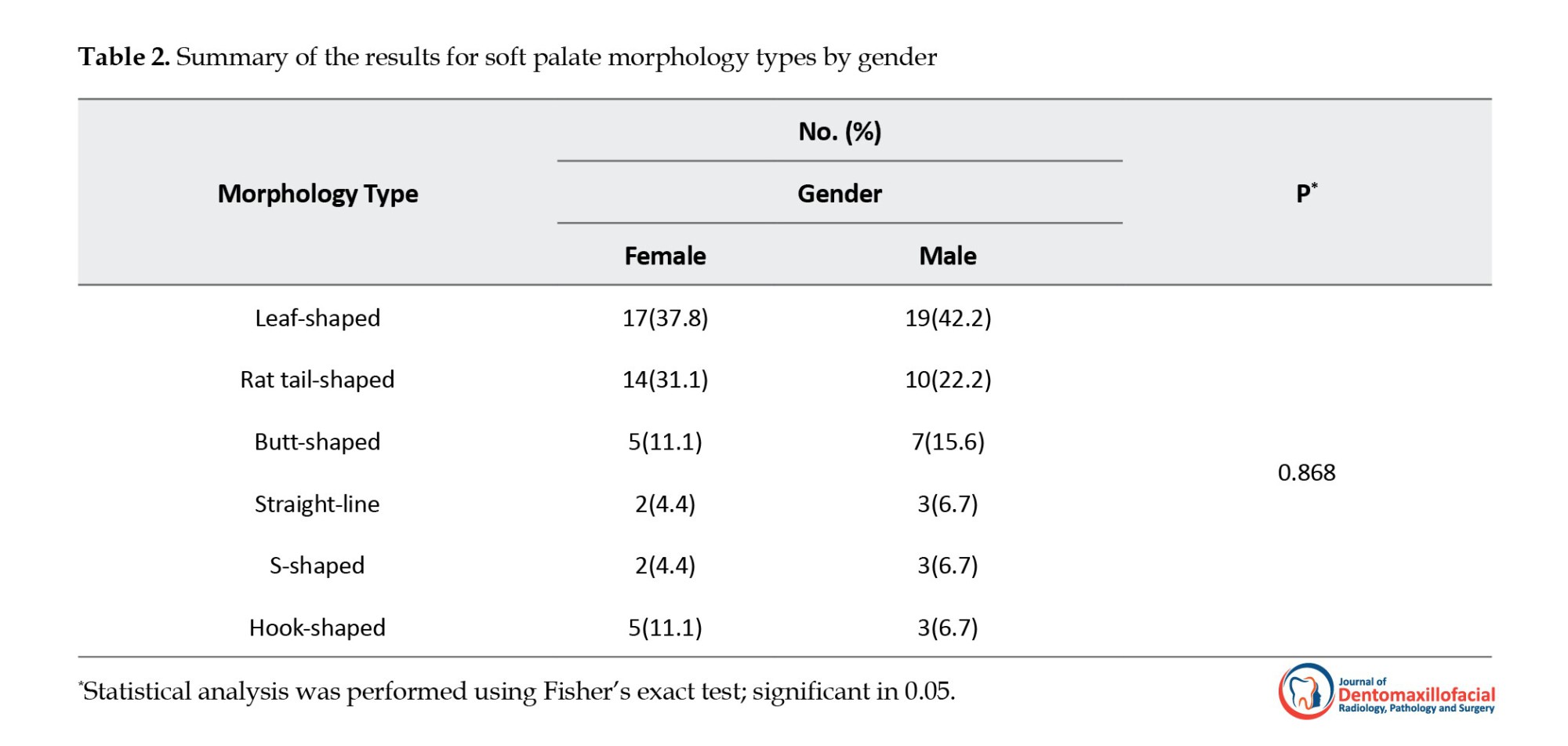
In accordance with Fisher’s exact test, there was no significant relationship between gender and morphology type (P=0.868; Table 2).
To analyze the relationship between morphology type and patient age group, Fisher’s exact test was used, and the results are presented in Table 3.
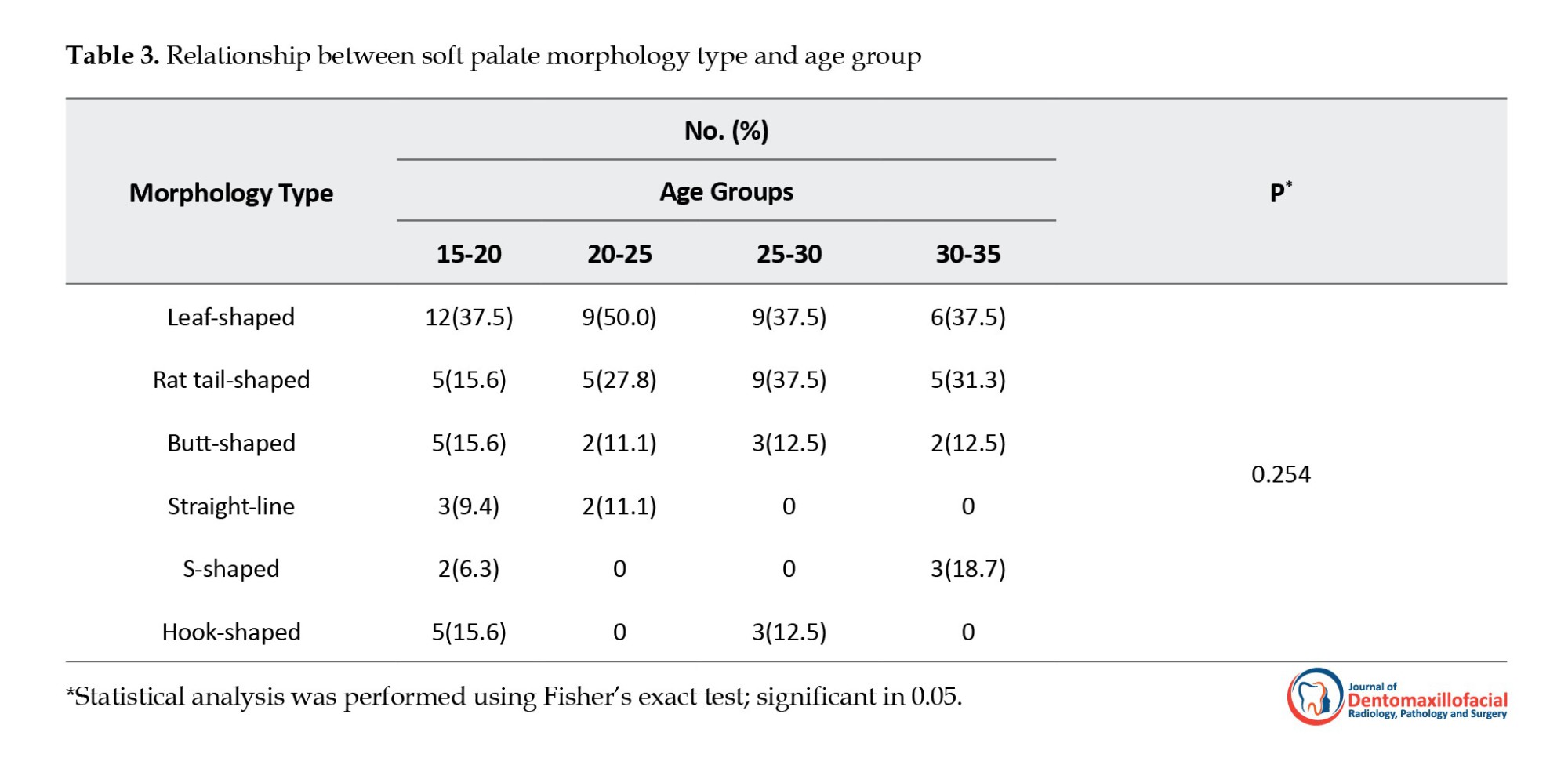
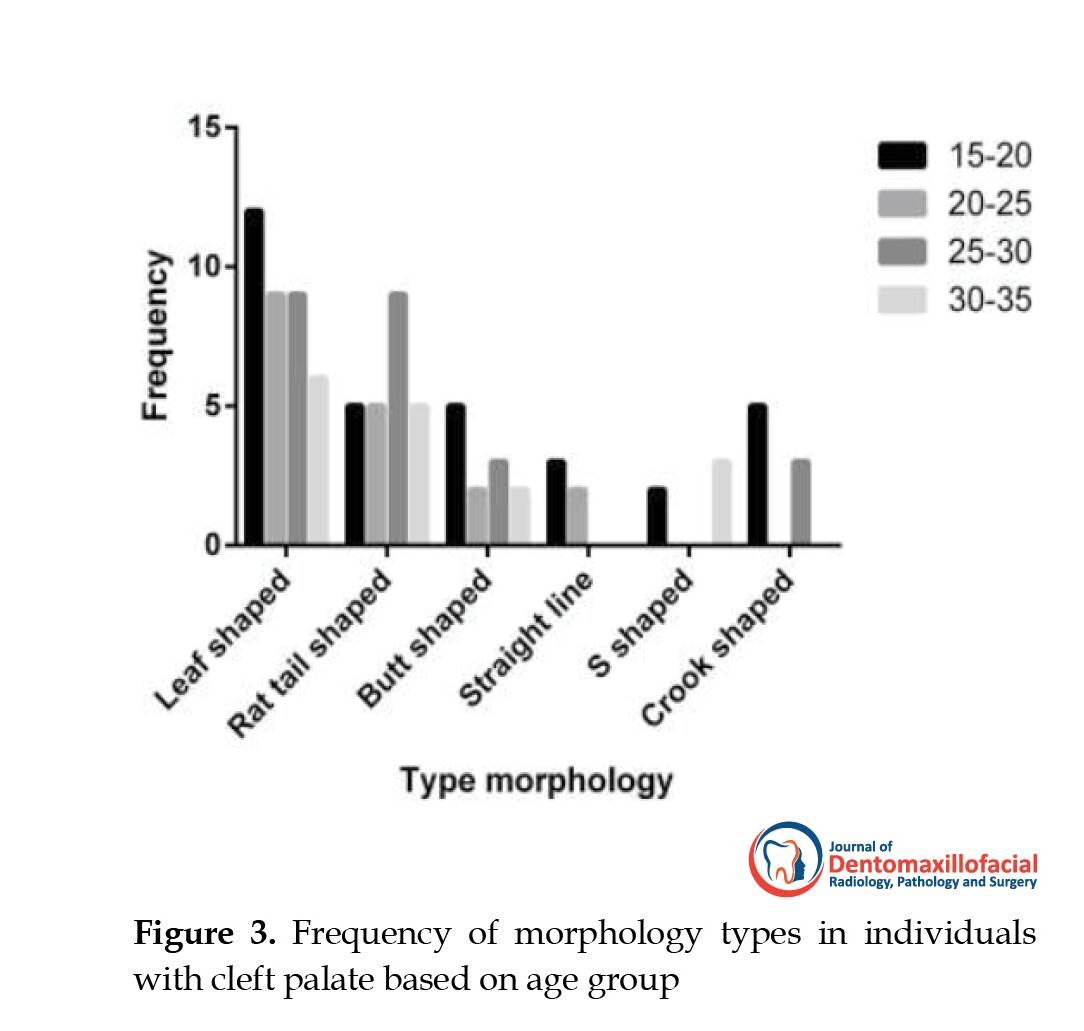
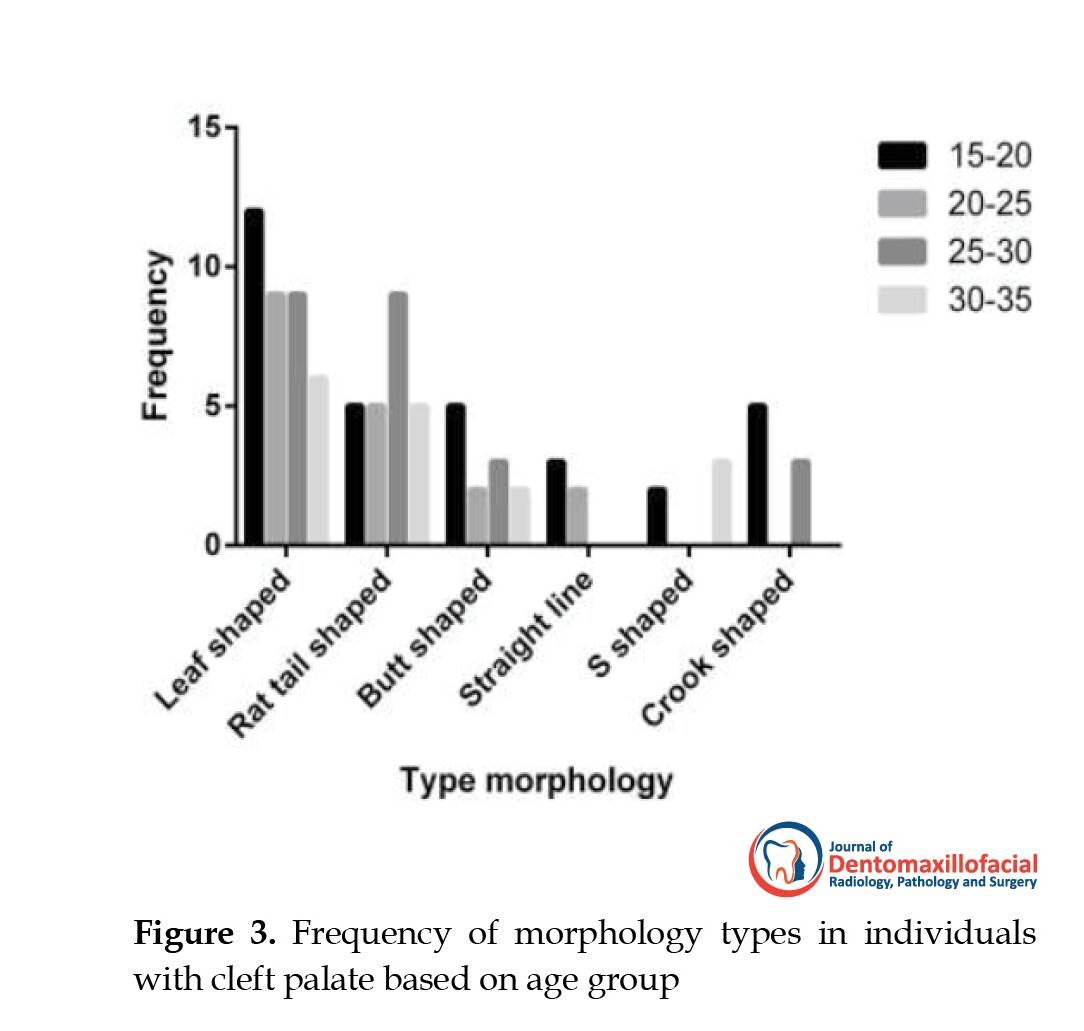
Figure 3 demonstrates the distribution of morphology types across age groups, which followed a relatively uniform pattern. As shown, there was no significant association between age group and morphology type (P=0.254; Table 3).
4. Discussion
The present study aimed to investigate the prevalence of different soft palate morphologies in patients with cleft palate who were referred to the dental schools of Guilan University of Medical Sciences between 2017 and 2019. Among the 90 participants, 45(50.0%) were female and 45(50.0%) were male. The age distribution revealed that the largest proportion of participants was in the 15–20-year age group, comprising 35.6% (32 individuals), followed by the 20–25, 25–30, and 30–35-year age groups, accounting for 20.0% (18 individuals), 26.7% (24 individuals), and 17.7% (16 individuals), respectively. Analysis of soft palate morphology, classified according to the You classification, indicated that the most common type was the leaf-shaped palate, observed in 40% (36 individuals). This was followed by the rat tail shaped (26.7%, 24 individuals), butt shaped (13.3%, 12 individuals), hook-shaped (8.8%, 8 individuals), straight line and s-shaped each one (5.6%, 5 individuals) morphologies.
Clinically, the predominance of the leaf-shaped soft palate in patients with cleft palate suggested a potential association with VPD risk. Since the morphology of the soft palate influences velopharyngeal closure efficiency, recognizing the leaf-shaped pattern as predominant may aid clinicians in predicting VPD severity and tailoring early interventions. This anatomical insight can guide surgical planning by informing the choice of repair techniques aimed at optimizing velar length and mobility to improve speech outcomes. Therefore, assessing soft palate morphology preoperatively can enhance personalized treatment strategies and improve functional prognosis in cleft palate management (24).
Ismail et al. (25) assessed the cephalometric association between various soft palate morphologies and different growth patterns and age groups in patients with skeletal class I, II, and III malocclusion. The study included 96 males and 286 females, aged 11 to 30 years. All patients were classified according to their skeletal malocclusion type. The obtained results revealed that leaf-shaped soft palate was the most prevalent morphology (43.2%), while straight-line shape was the least common (2.9%) which was consistent with the results of our study. Also, the leaf-shaped soft palate was the most frequent type across all skeletal malocclusion classes, growth patterns, and in both genders. Therefore, they found a significant association between soft palate morphology and both skeletal malocclusion type and gender. However, no significant association was observed between soft palate morphology and growth pattern.
Dahal et al. (26) investigated the morphological variations of the soft palate among patients. The observed morphological types of the soft palate were as follows: Rat-tail (42.4%), leaf-shaped (40.8%), butt-shaped (8.9 %), straight-line (4.7%), s-shaped (1.9%), and hook-shaped (0.9%). Among males, the distribution was rat-tail (44.4%), leaf-shaped (41.1%), butt-shaped (8.4%), straight-line (3.9%), s-shaped (1.3%), and hook-shaped (0.6%). In females, the frequencies were rat tail-shaped (40.6%), leaf-shaped (40.6%), butt-shaped (9.5%), straight-line (5.6%), s-shaped (2.5%), and hook-shaped (1.2%). The most frequently observed morphological shape in this study is inconsistent with our findings. Hence, they concluded that, the Rat-tail form was the most prevalent soft palate morphology, followed by the leaf-shaped type in both sexes, while the hook-shaped form was the least common. No evidence of sexual dimorphism was found in the distribution of soft palate types.
Chattopadhyay et al. (27) aimed to investigate the diverse radiographic morphologies of the soft palate using digital lateral cephalometry and evaluated the differences in morphological types across gender groups. Among the 300 patients, six distinct types of soft palate morphology were identified. The leaf-shaped (52%) and rat-tail shaped (25%) were the most prevalent, followed by straight-line shape (9.3%), hook appearance (7.3%), butt-like (3.3%), and s-shaped/distorted soft palate (3%). They concluded that, the soft palate can be broadly classified into six morphological types. This classification enhances our understanding of velar morphology in the median sagittal plane and serves as a valuable reference for research into velopharyngeal closure in individuals with cleft palate, obstructive sleep apnea, and other related conditions. In our study, the leaf-shaped palate emerged as the most prevalent morphology. This was followed by the rat tail-shape, butt-shape, hook-shape, respectively. Also, straight-line and s-shaped types were the least common.
Subramaniam et al. (28) evaluated the morphological diversity of the soft palate in 200 individuals. The results showed that the rat tail-shaped soft palate was the most common type (40%), while the butt-shaped type was the least common (2%) in both genders. In this study, neither the most frequent nor the least frequent soft palate types matched the findings of our research. These differences may be attributed to variations in ethnicity, geographic location, and sample size between the studies.
Samdani et al. (23) conducted a study in the relationship between various soft palate shapes and types of malocclusion in both genders. The study consisted of 250 individuals aged 14 to 28 years and all participants were assessed for the type of malocclusion, and the morphology of the soft palate was evaluated on digital lateral cephalograms, classified according to the six patterns described in the You classification. The results showed that the rat tail-shaped soft palate was the most frequent (37.2%), while the s-shaped soft palate had the lowest frequency (6.8%) in both genders. Regarding the least common type, these findings were consistent with our study; however, in our study, the leaf-shaped soft palate was the most prevalent, which differs from their results.
Verma et al. (29), investigated variations of soft palate morphology in 300 subjects aged between 15 and 45 years (mean age 31.32). This study examined soft palate types on lateral cephalograms and analyzed their correlation with gender and age groups, including the 15–35 age range studied in our research. The most frequent soft palate type found was leaf-shaped (48.7%), consistent with the prevalence found in our study. The study further explored relationships between soft palate morphology and anatomical measurements relevant to velopharyngeal closure.
The present study has several limitations. It was conducted at a single center, which may limit the generalizability of the findings. Selection bias is possible due to the recruitment method used. The use of 2D imaging restricts the ability to fully assess three-dimensional anatomical details. Additionally, functional assessment of the patients was not included, limiting the evaluation of clinical implications.
Future research should focus on investigating soft palate morphology using advanced 3D imaging techniques such as cone-beam computed tomography (CBCT) or magnetic resonance imaging (MRI) to capture detailed spatial anatomy. Including functional assessments like velopharyngeal closure evaluation through nasoendoscopy and nasometry would enhance understanding of the clinical implications of morphological variations. Additionally, exploring soft palate morphology differences across various cleft types and patients’ surgical repair histories can provide insights into the impact of treatment on velar anatomy. Such studies would address the limitations of 2D imaging and lack of functional data in the present study, advancing comprehensive cleft palate assessment.
5. Conclusions
The present study demonstrated that the leaf-shaped soft palate is the most prevalent morphology among patients with cleft palate, followed by rat-tail and butt-shaped types, while the straight-line and s-shaped types were least frequent. No significant associations were found between soft palate morphology and gender or age group. These findings are consistent with some previous studies but differ from others, indicating variability possibly due to ethnic and geographic factors. Clinically, understanding these morphological patterns can aid in tailored treatment planning and surgical interventions.
Ethical Considerations
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.443).
Funding
The present study was financially supported by Guilan University of Medical Sciences, Rasht, Iran.
Author's Contributions
Hamidreza Sharifipour Chokami: Conceptualization, Methodology Farzaneh Ostovarrad: Methodology, Data Curation Pedram Javidi: Supervision, Writing-Review and Editing Rasoul Tabari Khomeiran: Formal Analysis, Data Curation Amirreza Rostami: Investigation, Visualization, Writing-Original draft.
Conflict of Interest
The authors declared no conflict of interest.
Availability of Data and Material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
The authors thank Guilan University of Medical Sciences, Rasht, Iran, for the support.
References
Facial development initiates during the fourth week of embryogenesis with the emergence of medial nasal prominences, lateral nasal prominences, and maxillary prominences. Cleft lip arises from incomplete fusion of the medial nasal prominences (either with each other or the maxillary prominences), whereas cleft palate results from failed fusion of the palatal shelves (typically between weeks 8–12 of gestation) (1, 2).
The soft palate, a posterior fibromuscular extension of the palate connected to the posterior margin of the hard palate, comprises the levator veli palatini, tensor veli palatini, palatoglossus, palatopharyngeus, and musculus uvulae. It plays a vital role in swallowing, breathing, and speech (3). Dysfunction of the soft palate can result from various factors, including cleft lip and palate, enlarged adenoids, obstructive sleep apnea syndrome (OSAS), snoring, poorly maintained maxillary dentures, and craniofacial skeletal malocclusions. Understanding the normal anatomy and morphological variations of the soft palate is crucial for diagnosing and effectively managing these conditions (4, 5).
Cleft palate, a congenital disorder influenced by geographic, racial, and socioeconomic factors, has a global prevalence of 1 in 500–2,500 live births. More specific epidemiological data indicate that orofacial clefts overall, including cleft palate, occur in about 1 in 1,000 to 1,500 live births globally, which aligns with the general prevalence estimates often cited (6, 7). Patients often experience swallowing difficulties, speech impairments, and aesthetic concerns, necessitating surgical and prosthetic interventions to improve function and psychosocial well-being (8, 9).
Velopharyngeal dysfunction (VPD) is a primary speech complication in cleft palate patients. Insufficient soft palate mobility impairs its seal with the posterior pharyngeal wall, causing hypernasality and articulation disorders (10). It refers to the impaired function of the movable structures responsible for controlling the velopharyngeal sphincter. Approximately 30 % of patients who undergo cleft palate repair surgery require secondary surgical intervention due to persistent VPD. Understanding the normal anatomy and physiology of the velopharyngeal mechanism is the essential first step for an accurate diagnosis and effective treatment of children born with cleft lip and palate. The primary function of the velopharyngeal mechanism is to create a tight seal between the soft palate and the pharyngeal walls, thereby separating the oral and nasal cavities for various functions, including speech.
Velopharyngeal closure is accomplished through the coordinated contraction of several muscles, including the levator veli palatini, musculus uvulae, superior pharyngeal constrictor, palatopharyngeus, palatoglossus, and salpingopharyngeus (11, 12).
The primary goal of palatoplasty is to restore natural anatomy. Theoretically, palatoplasty improves the functional dynamics of the soft palate and pharyngeal walls by correcting dysmorphology in both the levator veli palatini and palatopharyngeus muscles (13). Pre- and postoperative anatomical assessments, along with short- and long-term outcome evaluations, enhance understanding of how different palatoplasty techniques influence soft palate structure. This is critical for optimizing velopharyngeal function, which underpins normal speech (14).
The Need’s ratio (soft palate length/pharyngeal depth) serves as a diagnostic tool for assessing velopharyngeal function. In individuals with normal anatomy, this ratio ranges between 0.6 and 0.7. Among the six soft palate morphologies classified by the You et al. classification system, type 6 (hook-shaped) demonstrates the highest soft-palate-to-pharyngeal-depth ratio (15, 16). Considering this issue, examining the type of soft palate morphology in patients with cleft palate can help in the early diagnosis and prevention of surgery caused by VPD. Deepa et al. (17) demonstrated morphological variations of the soft palate in the Indian population and identified multiple shapes such as rat-tail, butt-shape, and leaf-shape, with Rat-tail being the most common. It highlights no significant gender differences in soft palate types but notes variations in velar length with age and sex. Some shapes, like hook-shaped, may increase the risk of velopharyngeal insufficiency or sleep apnea.
Lateral cephalometric radiography is one of the most common extraoral radiographs after panoramic imaging, and it is applied in surgery and orthodontics treatment planning. It is used to measure anatomical distances and classify patients based on craniofacial morphology. As a standard diagnostic tool, it supports craniofacial assessment, treatment planning, progress monitoring, and outcome evaluation (18, 19). However, this technique projects three-dimensional craniofacial structures onto two-dimensional images, complicating accurate measurements even with optimal patient positioning (20). The main advantage of this technique is that the images obtained can be compared across different times and locations, allowing for the monitoring of growth, development, and treatment progress (21).
The soft palate has different morphologies in various diseases. Therefore, determining the different normal shapes of the soft palate in patients helps in the diagnosis and successful treatment of many complex cases and different diseases (22). There is a significant knowledge gap regarding the detailed morphological characteristics of the soft palate in cleft palate patients within the regional population, as no prior studies have specifically examined soft palate morphology among cleft palate patients in Guilan or similar regional settings. This lack of localized morphological data limits the understanding needed for tailored diagnosis and treatment planning in this population. Therefore, this study aimed to determine the frequency of soft palate morphology types in individuals with cleft palate among patients attending the dental schools of Guilan University of Medical Sciences from 2017-2019 using accessible lateral cephalometric radiographs.
2. Materials and Methods
This retrospective cross-sectional descriptive study was conducted on lateral cephalometric radiographs of 90 patients with isolated cleft palate who presented to the dental school at Guilan University of Medical Sciences from 2017 to 2019. The patients had cleft palate based on radiographic images. Automatic exposure settings with 60-90 kVp were used by the device to optimize the exposure conditions for each patient.
The required sample size was calculated to be n=89 based on a single proportion formula (Equation 1), assuming a 95% confidence level, 80% power, and an anticipated prevalence of 50% with a precision of 10%. To compensate for possible dropouts and missing data, the sample size was increased to 90 participants (23).
The sampling method of the study can be formally described as a systematic sampling approach with a reverse chronological order of selection. Specifically, lateral cephalometric radiographs of patients with cleft palate who met the inclusion criteria were systematically reviewed starting from the most recent radiographs and moving backward to older radiographs until the predetermined sample size of 89 was reached. This method ensured up-to-date data while maintaining a representative sample within the defined study period from 2017 to 2019. Only one radiograph per patient was included, duplicates were excluded, and radiographs with suboptimal quality or prior surgical intervention were omitted to enhance data validity. The rationale for reverse chronological selection is typically to capture the most current clinical presentations and imaging quality while avoiding selection bias inherent to arbitrary sampling. Observers were blinded to demographic details (age and sex) to reduce classification bias.
All lateral cephalograms were obtained using a Soredex Cranex (Helsinki, Finland) with cephalostat under standardized conditions. The patient’s head must be properly positioned with no rotation or tilt, maintaining the midsagittal plane perpendicular to the floor to avoid cephalometric distortion. The image must demonstrate clear visualization of critical anatomical landmarks with sharp contrast and no motion artifacts. Proper occlusion of the teeth is essential to allow accurate skeletal and dental analysis. Images must be free from external artifacts or obstructions that could interfere with interpretation. In the present study, any radiographs showing positioning inaccuracies such as head rotation beyond acceptable limits, poor image clarity, or suboptimal exposure conditions were excluded from analysis to maintain data quality. Manual analysis was performed using a negatoscope by one maxillofacial radiologist and one orthodontist, using tracing paper. The study employed the You et al. classification system (15) for soft palate morphology, comprising six types: The leaf-shaped form, in which the mid-portion is elevated toward the oral or nasal cavities; the rat-tail shaped type, characterized by anterior swelling with a distinct narrowing at the free edge; the butt-shaped form, which is short and wide with relatively uniform thickness; the straight-line type, showing a flat and planar configuration; the s-shaped (distorted soft palate), which presents an abnormal curvature resembling the letter “S”; and finally the hook-shaped form, where the posterior segment is curved anterosuperiorly, resembling a hook.
In cases where the morphology of the soft palate was ambiguous or borderline, these instances were managed through a consensus decision process between the two observers—a maxillofacial radiologist and an orthodontist—who independently analyzed the lateral cephalometric radiographs. When disagreement occurred on classification using the You et al. system (15), the observers reviewed the cases jointly to discuss the features and reach a mutual agreement. This approach ensured the reliability and accuracy of morphological classification by minimizing subjective bias and improving diagnostic consistency in borderline cases.
The inter-rater and intra-rater reliability for soft palate morphology classification were assessed using Cohen’s kappa coefficient, with values indicating excellent agreement. Cohen’s kappa was calculated by comparing the observed agreement between raters to the expected agreement by chance, expressed with a 95% confidence interval (CI). Values above 0.80 were interpreted as near-perfect agreement. Any classification disagreements were resolved through consensus discussions and joint image review to ensure consistent and reliable interpretation. This rigorous reliability assessment supports the robustness of the morphological data reported in this study. The descriptive analyses employed mean, frequency percentage, standard deviation, minimum, and maximum values. Statistical analysis was performed using Fisher’s exact test. Data processing was executed via SPSS software, version 19 and statistical significance was considered at 0.05.
3. Results
Based on the obtained results from Table 1, the number of participants in the study was equal in terms of gender. Moreover, the highest frequency is observed in the 15–20-year age group, comprising 32 individuals (35.6%), while the lowest frequency is found in the 30–35-year age group, with 16 individuals (17.7%).
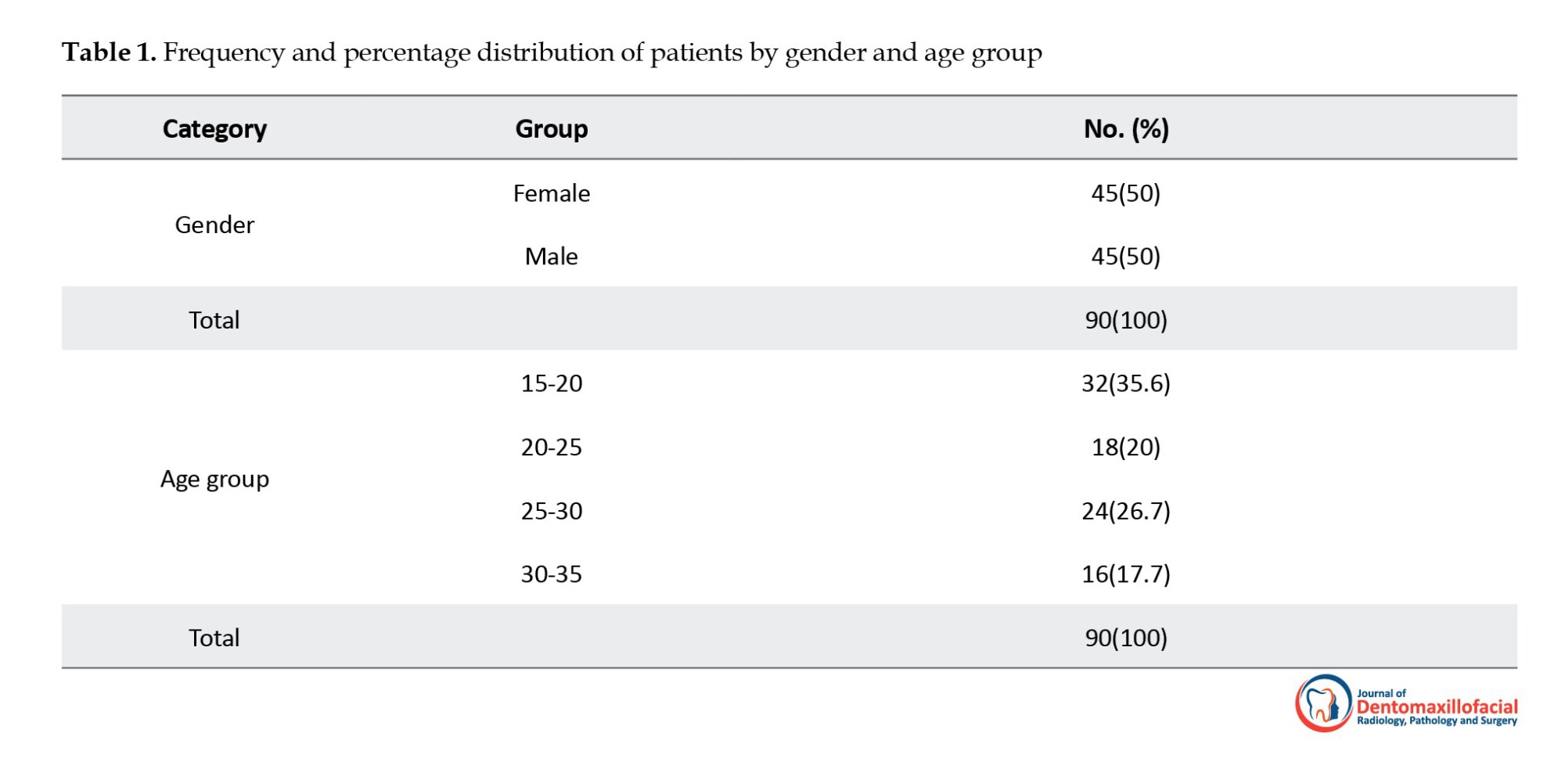
Figure 1 represents the frequency distribution of different soft palate morphology types, based on You et al. (15) classification system among individuals with cleft palate who attended dental schools at Guilan University of Medical Sciences. The results indicate that the leaf-shaped type had the highest frequency, with 36 cases (40%), while the straight-line and s-shaped had the lowest frequency, with 5 cases (5.6%). Figure 2 illustrates the distribution of morphology types by gender, showing similar patterns in males and females, with no remarkable differences.
In accordance with Fisher’s exact test, there was no significant relationship between gender and morphology type (P=0.868; Table 2).
To analyze the relationship between morphology type and patient age group, Fisher’s exact test was used, and the results are presented in Table 3.
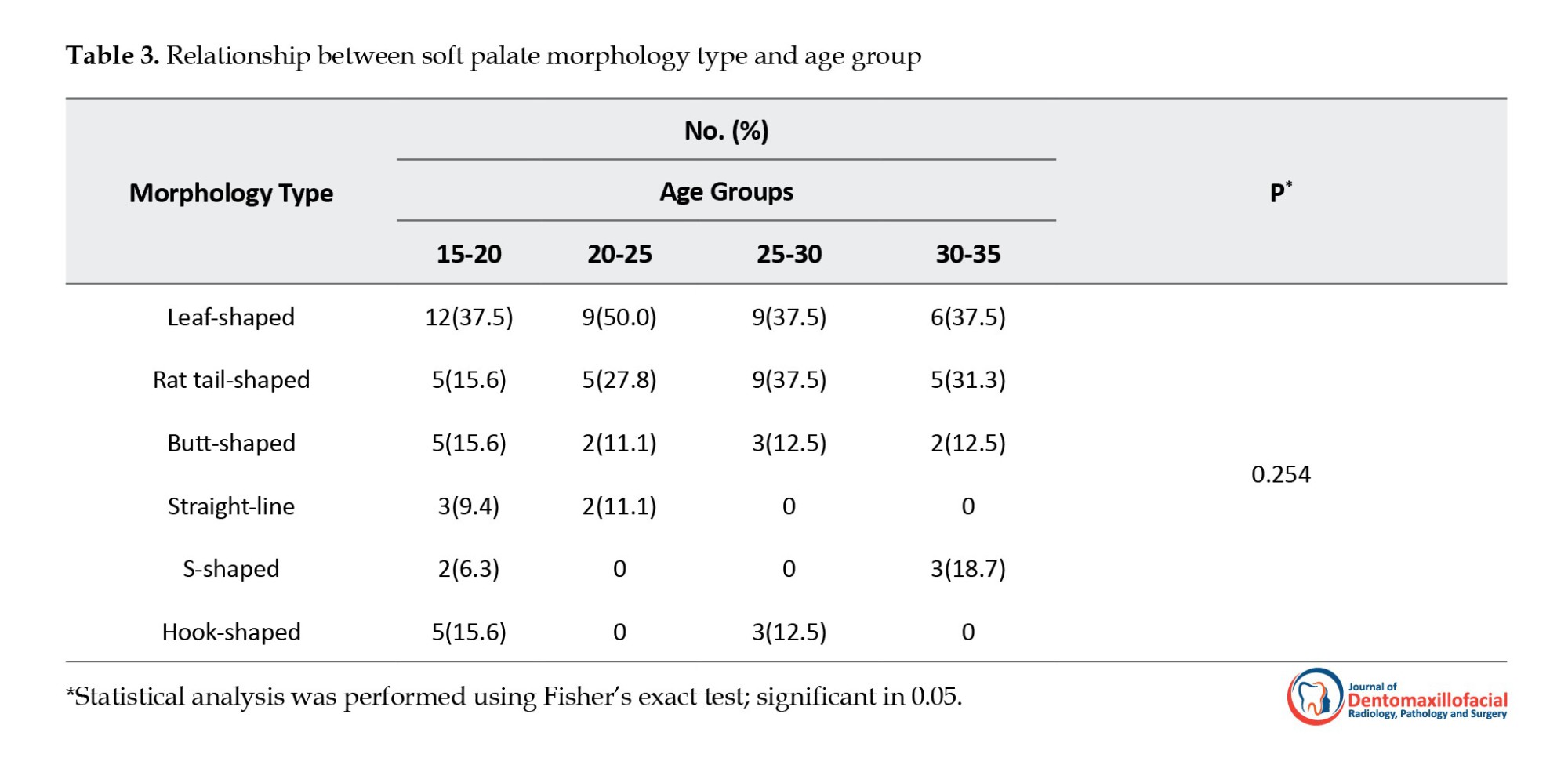
Figure 3 demonstrates the distribution of morphology types across age groups, which followed a relatively uniform pattern. As shown, there was no significant association between age group and morphology type (P=0.254; Table 3).
4. Discussion
The present study aimed to investigate the prevalence of different soft palate morphologies in patients with cleft palate who were referred to the dental schools of Guilan University of Medical Sciences between 2017 and 2019. Among the 90 participants, 45(50.0%) were female and 45(50.0%) were male. The age distribution revealed that the largest proportion of participants was in the 15–20-year age group, comprising 35.6% (32 individuals), followed by the 20–25, 25–30, and 30–35-year age groups, accounting for 20.0% (18 individuals), 26.7% (24 individuals), and 17.7% (16 individuals), respectively. Analysis of soft palate morphology, classified according to the You classification, indicated that the most common type was the leaf-shaped palate, observed in 40% (36 individuals). This was followed by the rat tail shaped (26.7%, 24 individuals), butt shaped (13.3%, 12 individuals), hook-shaped (8.8%, 8 individuals), straight line and s-shaped each one (5.6%, 5 individuals) morphologies.
Clinically, the predominance of the leaf-shaped soft palate in patients with cleft palate suggested a potential association with VPD risk. Since the morphology of the soft palate influences velopharyngeal closure efficiency, recognizing the leaf-shaped pattern as predominant may aid clinicians in predicting VPD severity and tailoring early interventions. This anatomical insight can guide surgical planning by informing the choice of repair techniques aimed at optimizing velar length and mobility to improve speech outcomes. Therefore, assessing soft palate morphology preoperatively can enhance personalized treatment strategies and improve functional prognosis in cleft palate management (24).
Ismail et al. (25) assessed the cephalometric association between various soft palate morphologies and different growth patterns and age groups in patients with skeletal class I, II, and III malocclusion. The study included 96 males and 286 females, aged 11 to 30 years. All patients were classified according to their skeletal malocclusion type. The obtained results revealed that leaf-shaped soft palate was the most prevalent morphology (43.2%), while straight-line shape was the least common (2.9%) which was consistent with the results of our study. Also, the leaf-shaped soft palate was the most frequent type across all skeletal malocclusion classes, growth patterns, and in both genders. Therefore, they found a significant association between soft palate morphology and both skeletal malocclusion type and gender. However, no significant association was observed between soft palate morphology and growth pattern.
Dahal et al. (26) investigated the morphological variations of the soft palate among patients. The observed morphological types of the soft palate were as follows: Rat-tail (42.4%), leaf-shaped (40.8%), butt-shaped (8.9 %), straight-line (4.7%), s-shaped (1.9%), and hook-shaped (0.9%). Among males, the distribution was rat-tail (44.4%), leaf-shaped (41.1%), butt-shaped (8.4%), straight-line (3.9%), s-shaped (1.3%), and hook-shaped (0.6%). In females, the frequencies were rat tail-shaped (40.6%), leaf-shaped (40.6%), butt-shaped (9.5%), straight-line (5.6%), s-shaped (2.5%), and hook-shaped (1.2%). The most frequently observed morphological shape in this study is inconsistent with our findings. Hence, they concluded that, the Rat-tail form was the most prevalent soft palate morphology, followed by the leaf-shaped type in both sexes, while the hook-shaped form was the least common. No evidence of sexual dimorphism was found in the distribution of soft palate types.
Chattopadhyay et al. (27) aimed to investigate the diverse radiographic morphologies of the soft palate using digital lateral cephalometry and evaluated the differences in morphological types across gender groups. Among the 300 patients, six distinct types of soft palate morphology were identified. The leaf-shaped (52%) and rat-tail shaped (25%) were the most prevalent, followed by straight-line shape (9.3%), hook appearance (7.3%), butt-like (3.3%), and s-shaped/distorted soft palate (3%). They concluded that, the soft palate can be broadly classified into six morphological types. This classification enhances our understanding of velar morphology in the median sagittal plane and serves as a valuable reference for research into velopharyngeal closure in individuals with cleft palate, obstructive sleep apnea, and other related conditions. In our study, the leaf-shaped palate emerged as the most prevalent morphology. This was followed by the rat tail-shape, butt-shape, hook-shape, respectively. Also, straight-line and s-shaped types were the least common.
Subramaniam et al. (28) evaluated the morphological diversity of the soft palate in 200 individuals. The results showed that the rat tail-shaped soft palate was the most common type (40%), while the butt-shaped type was the least common (2%) in both genders. In this study, neither the most frequent nor the least frequent soft palate types matched the findings of our research. These differences may be attributed to variations in ethnicity, geographic location, and sample size between the studies.
Samdani et al. (23) conducted a study in the relationship between various soft palate shapes and types of malocclusion in both genders. The study consisted of 250 individuals aged 14 to 28 years and all participants were assessed for the type of malocclusion, and the morphology of the soft palate was evaluated on digital lateral cephalograms, classified according to the six patterns described in the You classification. The results showed that the rat tail-shaped soft palate was the most frequent (37.2%), while the s-shaped soft palate had the lowest frequency (6.8%) in both genders. Regarding the least common type, these findings were consistent with our study; however, in our study, the leaf-shaped soft palate was the most prevalent, which differs from their results.
Verma et al. (29), investigated variations of soft palate morphology in 300 subjects aged between 15 and 45 years (mean age 31.32). This study examined soft palate types on lateral cephalograms and analyzed their correlation with gender and age groups, including the 15–35 age range studied in our research. The most frequent soft palate type found was leaf-shaped (48.7%), consistent with the prevalence found in our study. The study further explored relationships between soft palate morphology and anatomical measurements relevant to velopharyngeal closure.
The present study has several limitations. It was conducted at a single center, which may limit the generalizability of the findings. Selection bias is possible due to the recruitment method used. The use of 2D imaging restricts the ability to fully assess three-dimensional anatomical details. Additionally, functional assessment of the patients was not included, limiting the evaluation of clinical implications.
Future research should focus on investigating soft palate morphology using advanced 3D imaging techniques such as cone-beam computed tomography (CBCT) or magnetic resonance imaging (MRI) to capture detailed spatial anatomy. Including functional assessments like velopharyngeal closure evaluation through nasoendoscopy and nasometry would enhance understanding of the clinical implications of morphological variations. Additionally, exploring soft palate morphology differences across various cleft types and patients’ surgical repair histories can provide insights into the impact of treatment on velar anatomy. Such studies would address the limitations of 2D imaging and lack of functional data in the present study, advancing comprehensive cleft palate assessment.
5. Conclusions
The present study demonstrated that the leaf-shaped soft palate is the most prevalent morphology among patients with cleft palate, followed by rat-tail and butt-shaped types, while the straight-line and s-shaped types were least frequent. No significant associations were found between soft palate morphology and gender or age group. These findings are consistent with some previous studies but differ from others, indicating variability possibly due to ethnic and geographic factors. Clinically, understanding these morphological patterns can aid in tailored treatment planning and surgical interventions.
Ethical Considerations
This study was approved by the Ethics Committee of Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.443).
Funding
The present study was financially supported by Guilan University of Medical Sciences, Rasht, Iran.
Author's Contributions
Hamidreza Sharifipour Chokami: Conceptualization, Methodology Farzaneh Ostovarrad: Methodology, Data Curation Pedram Javidi: Supervision, Writing-Review and Editing Rasoul Tabari Khomeiran: Formal Analysis, Data Curation Amirreza Rostami: Investigation, Visualization, Writing-Original draft.
Conflict of Interest
The authors declared no conflict of interest.
Availability of Data and Material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
The authors thank Guilan University of Medical Sciences, Rasht, Iran, for the support.
References
- Hammond NL, Dixon MJ. Revisiting the embryogenesis of lip and palate development. Oral Dis. 2022; 28(5):1306-26. [DOI:10.1111/odi.14174] [PMID]
- Naini FB, Cobourne MT, Garagiola U, McDonald F, Wertheim D. Nasofacial angle and nasal prominence: A quantitative investigation of idealized and normative values. J Craniomaxillofac Surg. 2016; 44(4):446-52. [DOI:10.1016/j.jcms.2016.01.010] [PMID]
- Cho JH, Kim JK, Lee HY, Yoon JH. Surgical anatomy of human soft palate. Laryngoscope. 2013; 123(11):2900-4. [DOI:10.1002/lary.24067] [PMID]
- Helwany M, Rathee M. Anatomy, head and neck, palate. Treasure Island: StatPearls Publishing; 2023. [Link]
- Pham Q, Lentner M, Hu A. Soft palate injuries during orotracheal intubation with the videolaryngoscope. Ann Otol Rhinol Laryngol. 2017; 126(2):132-7. [DOI:10.1177/0003489416678008] [PMID]
- Applebaum SA, Aronson S, Termanini KM, Gosain AK. Evidence-based practices in cleft palate surgery. Plastic Reconstruct Surg. 2024; 153(2):448e-61e. [DOI:10.1097/PRS.0000000000011035] [PMID]
- Sakran KA, Yin J, Yang R, Elayah SA, Alkebsi K, Zhang S, et al. Early cleft palate repair by a modified technique without relaxing incisions. Cleft Palate Craniofac J. 2024; 61(4):646-53. [DOI:10.1177/10556656221135288] [PMID]
- Sakran KA, Wu M, Alkebsi K, Mashrah MA, Al‐Rokhami RK, Wang Y, et al. The sommerlad-furlow modified palatoplasty technique: Postoperative complications and implicating factors. Laryngoscope. 2023; 133(4):822-9. [DOI:10.1002/lary.30385] [PMID]
- Cheng X, Bo Z, Yin H, Yang K, Li J, Shi B. Age and preoperative velar closure ratio are significantly associated with surgical outcome of Furlow double-opposing Z-plasty in palatal re-repair. J Oral Maxillofac Surg. 2020; 78(3):431-9. [DOI:10.1016/j.joms.2019.09.023] [PMID]
- Chiang SN, Fotouhi AR, Grames LM, Skolnick GB, Snyder-Warwick AK, Patel KB. Buccal myomucosal flap repair for velopharyngeal dysfunction. Plast Reconstr Surg. 2023; 152(4):842-50. [DOI:10.1097/PRS.0000000000010443] [PMID]
- Espel JP, Hohman MH, Winters R. Cleft palate repair. Treasure Island: StatPearls Publishing; 2023. [Link]
- Nachmani A, Masalha M, Kassem F. Phonological profile of patients with velopharyngeal dysfunction and palatal anomalies. J Speech Lang Hear Res. 2021; 64(12):4649-63. [DOI:10.1044/2021_JSLHR-20-00652] [PMID]
- Sakran K, Liu R, Yu T, Al-Rokhami R, He D. A comparative study of three palatoplasty techniques in wide cleft palates. Int J Oral Maxillofac Surg. 2021; 50(2):191-7. [DOI:10.1016/j.ijom.2020.07.016] [PMID]
- Pang K, Pang E, Pang K, Rotenberg B. Anterior palatoplasty in the treatment of obstructive sleep apnoea-A systematic review. Acta Otorhinolaryngol Ital. 2017; 38(1):1-6. [DOI:10.14639/0392-100X-1641] [PMID]
- You M, Li X, Wang H, Zhang J, Wu H, Liu Y, et al. Morphological variety of the soft palate in normal individuals: A digital cephalometric study. Dentomaxillofac Radiol. 2008; 37(6):344-9. [DOI:10.1259/dmfr/55898096] [PMID]
- Preetha VM, Vardhan BH, Gopal KS, Lankupalli AS. Assessing the prevalence of velopharyngeal dysfunction and obstructive sleep apnea by correlating cone beam computed tomography parameters of soft palate with the stop bang questionnaire. J Indian Acad Oral Med Radiol. 2021; 33(3):294-300. [DOI:10.4103/jiaomr.jiaomr_81_21]
- Deepa V, Ramnarayan BK. Morphological varieties of soft palate in normal individuals, cleft palate patients and obstructive sleep apnea patients with reference to Indian population: A preliminary digital cephalometric study. World J Dent. 2015; 4(4):241-9. [DOI:10.5005/jp-journals-10015-1239]
- Icoz D, Kok H. Evaluation of sella turcica and maxilla morphometry of individuals with cleft lip and palate on lateral cephalometric radiographs. Eur J Ther. 2024; 30(5):580-8. [DOI:10.58600/eurjther2247]
- Ferrario VF, Sforza C, Miani A, Tartaglia G. Craniofacial morphometry by photographic evaluations. Am J Orthod Dentofacial Orthop. 1993; 103(4):327-37. [DOI:10.1016/0889-5406(93)70013-E] [PMID]
- Guinot‐Barona C, Alonso Pérez‐Barquero J, Galán López L, Barmak AB, Att W, Kois JC, et al. Cephalometric analysis performance discrepancy between orthodontists and an artificial intelligence model using lateral cephalometric radiographs. J Esthet Restor Dent.2024; 36(4):555-65. [DOI:10.1111/jerd.13156] [PMID]
- Hussain S, Mubeen I, Ullah N, Shah SSUD, Khan BA, Zahoor M, et al. Modern diagnostic imaging technique applications and risk factors in the medical field: A review. BioMed Res Int. 2022; 2022(1):5164970. [DOI:10.1155/2022/5164970] [PMID]
- Almoammar KA. Harnessing the power of artificial intelligence in cleft lip and palate: An in-depth analysis from diagnosis to treatment, a comprehensive review. Children. 2024; 11(2):140. [DOI:10.3390/children11020140] [PMID]
- Samdani D, Saigal A, Garg E. Correlation of morphological variants of soft palate and types of malocclusion: A digital lateral cephalometric study. J Indian Acad Oral Med Radiol. 2015; 27(3):366. [DOI:10.4103/0972-1363.170451]
- Gupta GS, Meghana HC, Shetty U, Rai DV, Rao PK, Kini R. Assessment of the morphology of soft palate by using cone-beam computed tomography. J Indian Acad Oral Med Radiol. 2022; 34(2):213-217. [DOI:10.4103/jiaomr.jiaomr_56_22]
- Ismail N, Shaikh A, Khan SA. Cephalometric association between various shapes of soft palate with different growth pattern and age groups in skeletal class I, II and III malocclusion. J Pak Dent Assoc. 2023; 32(3):85-90. [DOI:10.25301/JPDA.323.85]
- Dahal S, Gupta SP, Singh AK, Baral R, Giri A. The morphological variation of the soft palate in hospital visiting patients. J Nepal Health Res Counc. 2022; 20(1):229-233. [DOI:10.33314/jnhrc.v20i01.4044] [PMID]
- Chattopadhyay S, Arora R, Kishor A, Singh S, Alok A. Morphological variations of soft palate: A digital cephalometric study. J Pharm Negative Results. 2022; 13(8):4680-5. [Link]
- Subramaniam N, Muthukrishnan A. Assessment of various shapes of soft palate-a retrospective lateral cephalometric study. Res J Pharm Technol. 2018; 11(12):5233-7. [DOI:10.5958/0974-360X.2018.00954.X]
- Verma P, Verma KG, Kumaraswam KL, Basavaraju S, Sachdeva SK, Juneja S. Correlation of morphological variants of the soft palate and Need’s ratio in normal individuals: A digital cephalometric study. Image Sci Dent. 2014; 44(3):193-8. [DOI:10.5624/isd.2014.44.3.193] [PMID]
Type of Study: Original article |
Subject:
Radiology
Received: 2025/08/9 | Accepted: 2025/09/26 | Published: 2025/09/15
Received: 2025/08/9 | Accepted: 2025/09/26 | Published: 2025/09/15
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |