Fri, Apr 26, 2024
Volume 7, Issue 3 (9-2018)
2018, 7(3): 109-114 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Karbasi kheir M, Fathollahzadeh H. Assessment of Accessory Mental Foramen by Cone-beam Computerized Tomography. Journal title 2018; 7 (3) :109-114
URL: http://3dj.gums.ac.ir/article-1-322-en.html
URL: http://3dj.gums.ac.ir/article-1-322-en.html
1- Assistant professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Islamic Azad University of Isfahan (Khorasgan Branch), Isfahan, Iran. , mastoor28@yahoo.com
2- Assistant professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Arak University of Medical Sciences, Arak, Iran.
2- Assistant professor, Department of Oral and Maxillofacial Radiology, School of Dentistry, Arak University of Medical Sciences, Arak, Iran.
Full-Text [PDF 966 kb]
(660 Downloads)
| Abstract (HTML) (1917 Views)
Full-Text: (779 Views)
1. Introduction
he mental foramen is a bilateral opening in the anterolateral aspect of the mandibular body through which nerve endings such as mental nerve, arteries, and veins pass [1-4]. Any additional foramen, except mental foramen, in the body of the mandible is called Accessory Mental Foramen (AMF). AMF transfers the accessory branch of the mental nerve. It normally occurs singly, but up to 4 AMFs can appear on one side of the mandible. The separation of the mental nerve into several fasciculi before the development of mental foramen during the 12th week of intrauterine life causes the formation of accessory foramen(s) [3-17]. Studies have shown the different incidence of AMF among various ethnic groups [6-14]. Damaging the neurovascular bundle in AMF causes sensory disturbances and hemorrhages after surgical procedures [8, 14]. Although this anatomical variation is rare, the early detection of this structure through careful radiographic interpretation minimizes the risk of iatrogenic injury.
The presence of AMF has been already evaluated on dissection studies, surgical findings, conventional radiographs, spiral Computed Tomography (CT), and Cone-Beam CT (CBCT). However, the identification of AMF by the two-dimensional exams is difficult because AMF is usually smaller than 1.0mm. CBCT, which uses a lower patient dose than CT, has become established as a diagnostic tool to determine the anatomical variations [2-13]. Jaju et al. concluded that 3D reconstructions might help to identify the AMFs and differentiate them from nutritive foramina [9]. The objective of this study was the determination of the AMF using CBCT.
2. Materials and Methods
In this descriptive study, 180 CBCT images were selected by simple sampling method from a university data set. The images were taken from the patients for diagnostic purposes in the Department of Maxillofacial Radiology from 2010 to 2015. The inclusion criteria comprised the patients older than 18 years whose skeletal growth was completed (partially or fully edentulous and dentate patients), and the exclusion criteria consisted of patients with pathologic lesions in the mandible. Two maxillofacial radiologists examined the images to avoid misinterpretations caused by one radiologist. The images were observed on an LGLED computer viewer (E2042C, Korea) using Sirona Galelio’s software. All CBCT images were taken by Sirona Orthophos, GALILEOS version 1.7 (Sirona, Germany), with a flat-panel detector. The adjusted scan parameters were 85kVp and 10-42 mA, depending on the size of the patients. Exposure time was 14s, the effective exposure time was 2-6 s, and voxel size was 0.3×0.3×0.3 mm.
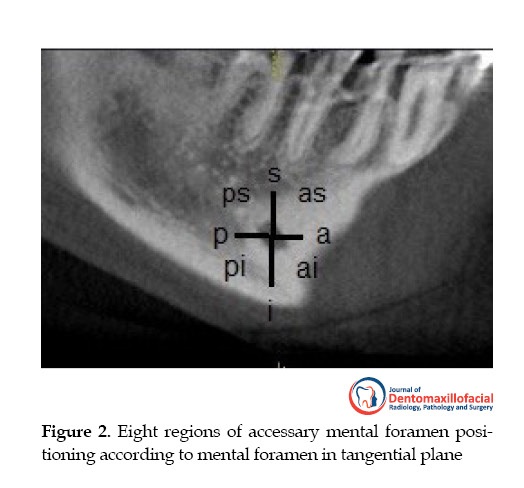
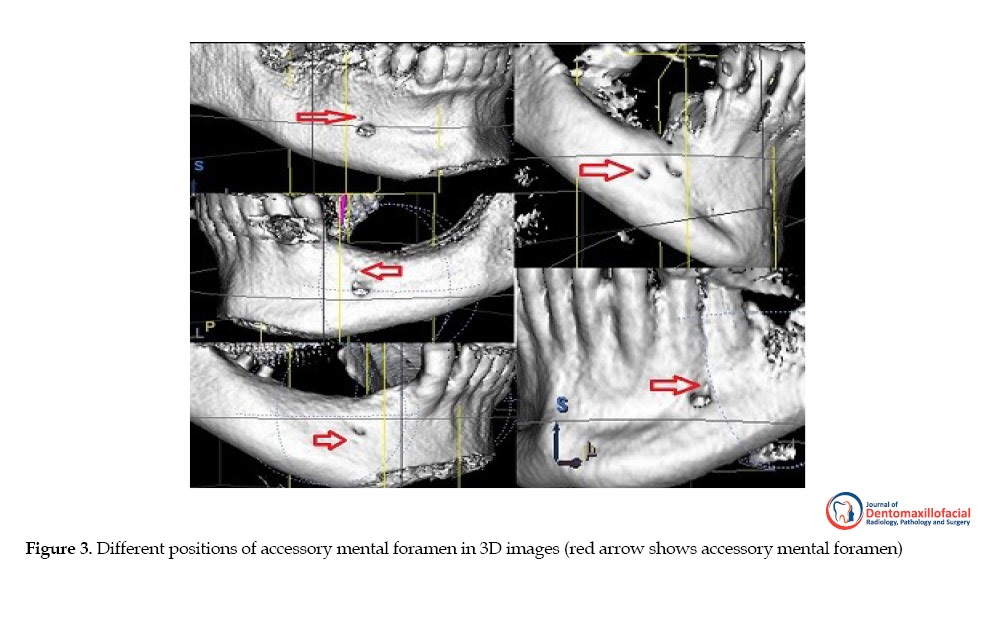
The CBCT images were analyzed in different sectional planes (tangential, cross-sectional, axial, and 3D). Right and left sides of all images were evaluated and then statically analyzed one by one. The location of the inferior alveolar nerve canal was determined from mandibular foramen to mental foramen employing the nerve option of Sirona Galelio’s software on tangential and cross-sectional slices. The AMF was checked in tangential and cross-sectional slices. Each one had a connection with the inferior alveolar canal in the cross-sectional slices and an opening in the buccal surface of the mandibular body Figure 1. The position of AMF was assessed on reconstructed 3D CBCT images or tangential images in eight regions of postero-superior, posterior, postero-inferior, superior, inferior, postero-anterior, anterior, and superior-antero-superior regions Figure 2.
he mental foramen is a bilateral opening in the anterolateral aspect of the mandibular body through which nerve endings such as mental nerve, arteries, and veins pass [1-4]. Any additional foramen, except mental foramen, in the body of the mandible is called Accessory Mental Foramen (AMF). AMF transfers the accessory branch of the mental nerve. It normally occurs singly, but up to 4 AMFs can appear on one side of the mandible. The separation of the mental nerve into several fasciculi before the development of mental foramen during the 12th week of intrauterine life causes the formation of accessory foramen(s) [3-17]. Studies have shown the different incidence of AMF among various ethnic groups [6-14]. Damaging the neurovascular bundle in AMF causes sensory disturbances and hemorrhages after surgical procedures [8, 14]. Although this anatomical variation is rare, the early detection of this structure through careful radiographic interpretation minimizes the risk of iatrogenic injury.
The presence of AMF has been already evaluated on dissection studies, surgical findings, conventional radiographs, spiral Computed Tomography (CT), and Cone-Beam CT (CBCT). However, the identification of AMF by the two-dimensional exams is difficult because AMF is usually smaller than 1.0mm. CBCT, which uses a lower patient dose than CT, has become established as a diagnostic tool to determine the anatomical variations [2-13]. Jaju et al. concluded that 3D reconstructions might help to identify the AMFs and differentiate them from nutritive foramina [9]. The objective of this study was the determination of the AMF using CBCT.
2. Materials and Methods
In this descriptive study, 180 CBCT images were selected by simple sampling method from a university data set. The images were taken from the patients for diagnostic purposes in the Department of Maxillofacial Radiology from 2010 to 2015. The inclusion criteria comprised the patients older than 18 years whose skeletal growth was completed (partially or fully edentulous and dentate patients), and the exclusion criteria consisted of patients with pathologic lesions in the mandible. Two maxillofacial radiologists examined the images to avoid misinterpretations caused by one radiologist. The images were observed on an LGLED computer viewer (E2042C, Korea) using Sirona Galelio’s software. All CBCT images were taken by Sirona Orthophos, GALILEOS version 1.7 (Sirona, Germany), with a flat-panel detector. The adjusted scan parameters were 85kVp and 10-42 mA, depending on the size of the patients. Exposure time was 14s, the effective exposure time was 2-6 s, and voxel size was 0.3×0.3×0.3 mm.
The CBCT images were analyzed in different sectional planes (tangential, cross-sectional, axial, and 3D). Right and left sides of all images were evaluated and then statically analyzed one by one. The location of the inferior alveolar nerve canal was determined from mandibular foramen to mental foramen employing the nerve option of Sirona Galelio’s software on tangential and cross-sectional slices. The AMF was checked in tangential and cross-sectional slices. Each one had a connection with the inferior alveolar canal in the cross-sectional slices and an opening in the buccal surface of the mandibular body Figure 1. The position of AMF was assessed on reconstructed 3D CBCT images or tangential images in eight regions of postero-superior, posterior, postero-inferior, superior, inferior, postero-anterior, anterior, and superior-antero-superior regions Figure 2.
Statistical analysis
Kappa coefficients were computed to evaluate the inter-observer agreement of the images taken by CBCT. We used the Fisher exact-test to examine the presence of AMF concerning the sex. Also, we employed the t-test to check the relationship between AMF and age on each side separately. Statistical significance was set at P<0.05.
3. Results
Out of 180 CBCT images, 84 belonged to men and 96 to women. The mean age of the patients was 48 years (SD=±13.9). Table 1 presents the frequency percentages of dentate, partially, and fully edentulous on both sides. The Kappa coefficient for an inter-observer agreement of CBCT images was 1.00 (P<0.001) with 100% agreement. The frequency of AMF was 3.3% (n=6) on the right side, 5.6% (n=10) on the left side, and 1.1% (n=2) on both sides. The results of the Fisher exact-test showed a significant difference between the right and left sides (P=0.03).
Kappa coefficients were computed to evaluate the inter-observer agreement of the images taken by CBCT. We used the Fisher exact-test to examine the presence of AMF concerning the sex. Also, we employed the t-test to check the relationship between AMF and age on each side separately. Statistical significance was set at P<0.05.
3. Results
Out of 180 CBCT images, 84 belonged to men and 96 to women. The mean age of the patients was 48 years (SD=±13.9). Table 1 presents the frequency percentages of dentate, partially, and fully edentulous on both sides. The Kappa coefficient for an inter-observer agreement of CBCT images was 1.00 (P<0.001) with 100% agreement. The frequency of AMF was 3.3% (n=6) on the right side, 5.6% (n=10) on the left side, and 1.1% (n=2) on both sides. The results of the Fisher exact-test showed a significant difference between the right and left sides (P=0.03).
In the right side, 4 (4.8%) men and 2 (2.1%) women and in the left side, 4 (4.8%) men and 6 (6.3%) women had AMF. The results of the Fisher exact-test did not show a significant difference between the presence of AMF and gender (right side P=0.42, left side P=0.73). The Mean±SD age of the patients with AMF on the right side was 54±17.94 years and on the left side was 52±14.75 years. The Mean±SD age of patients without AMF on the right side was 48±13.74 years and on the left side was 48±13.83 years. The results of t-test showed no significant difference between age and existence of the AMF (right side P=0.3, left side P=0.32).
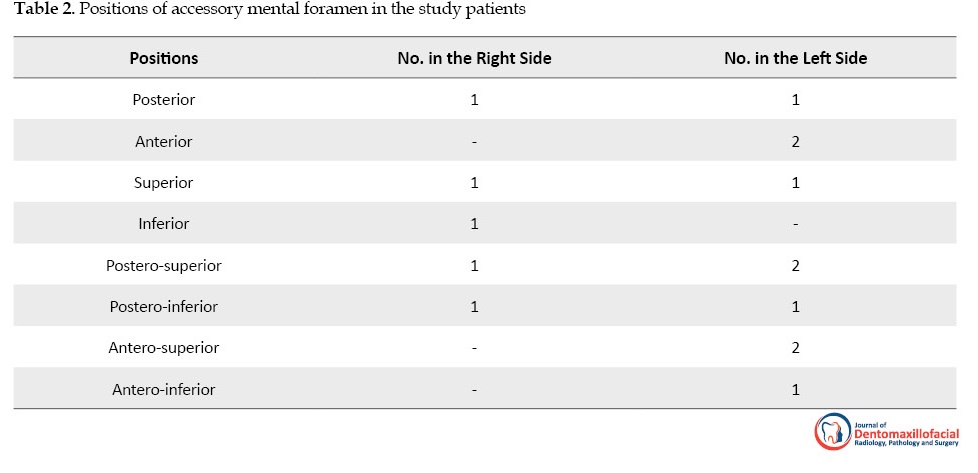
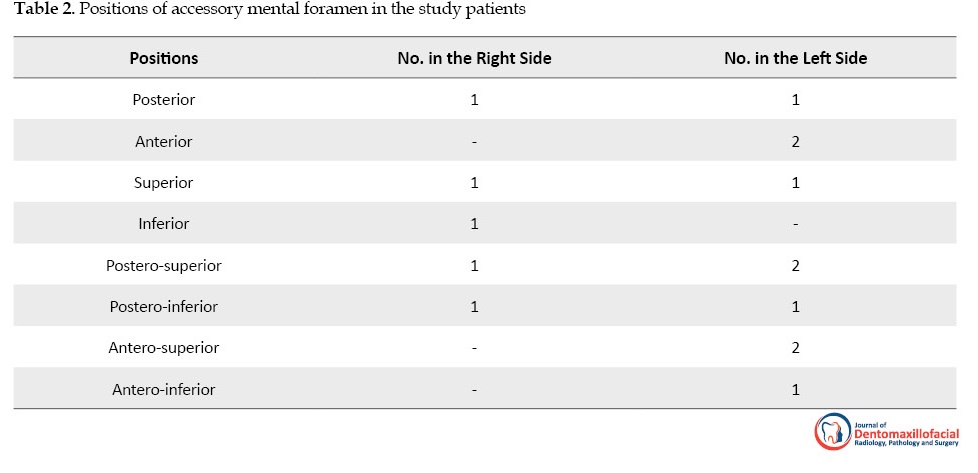
On the right side, five images had only one AMF, and one image sample had two AMFs in the anterior and anterior-superior positions. On the left side, however, all of the image samples had one AMF. Table 2 presents the position of AMF on the right and left sides in patients with one AMF.
On the right side, five images had only one AMF, and one image sample had two AMFs in the anterior and anterior-superior positions. On the left side, however, all of the image samples had one AMF. Table 2 presents the position of AMF on the right and left sides in patients with one AMF.
4. Discussion
The AMF is a rare variation in association with mental foramen. It carries a branch of the inferior alveolar nerve that emerges the mandibular canal from a different foramen and supplies the same area with the mental nerve. If left undetected, some neurovascular complications will happen during operations like implant placement, regional anesthesia, surgical correction of jaw deformities, and periapical surgery. Therefore, knowledge about this anatomic variation influences the treatment plan [3, 14].
As Torres et al. stated, it was important to differentiate an AMF from a nutrient foramen, which did not originate from the mandibular canal [2]. This study showed that it was easy to differentiate AMFs employing cross-sectional images of CBCT. Cross-sectional images show well the relation of AMF with mental nerve and inferior alveolar nerve canal.
The prevalence of AMF is between 1.4% and 12% and has not any predilection to side, age, and gender. However, the rate of AMF varies among different ethnic groups. For example it is 2.6% in French, 1.4% in White Americans, 5.7% in Black Americans, 1.5% in Asian-Indians, 9.0% in Pre-Columbian Nazca Indians, 3.3% in Greeks, 1.5% in Russians, 3.0% in Hungarians, 9.7% in Melanesians, 6.3% in Turkish, 8.4% in Indians, 3.6% in Egyptians, and 6.7%-12.5% in Japanese [6, 7, 9, 13, 15-18]. In this study, the incidence of AMF was 7.7%. Like other studies, no age and gender predilections were seen in the presence of AMF in this study [6, 17].
Avni Balcioglu et al. concluded that non-Caucasians might have a higher rate of AMF than Caucasians, which seemed to be in contrast with the present study [13]. Although most Iranians are Caucasian, they have shown a high prevalence of AMF similar to Japanese people. However, more studies with larger sample sizes are required to show its real incidence in Iranian population. Therefore, the sample size is as one of the limitations of this study. In another study on an Iranian population with fewer samples, the incidence of AMF is 5.1% which is similar to the present study; there were no gender and age predilections in the presence of AMF [11].
The most outstanding and novel feature in the present study, in contrast with Khojastepoor et al. study, was the classification of AMF position into eight regions [11]. Moreover, in the present study, the method of defining AMF is more accurate because of using cross-sectional images in combination with tangential and 3D images Figures 1, 2, 3. Khojastepoor et al. conducted their study on fewer samples, and did not examine the presence of AMF on the right and left sides [11].
The AMF is a rare variation in association with mental foramen. It carries a branch of the inferior alveolar nerve that emerges the mandibular canal from a different foramen and supplies the same area with the mental nerve. If left undetected, some neurovascular complications will happen during operations like implant placement, regional anesthesia, surgical correction of jaw deformities, and periapical surgery. Therefore, knowledge about this anatomic variation influences the treatment plan [3, 14].
As Torres et al. stated, it was important to differentiate an AMF from a nutrient foramen, which did not originate from the mandibular canal [2]. This study showed that it was easy to differentiate AMFs employing cross-sectional images of CBCT. Cross-sectional images show well the relation of AMF with mental nerve and inferior alveolar nerve canal.
The prevalence of AMF is between 1.4% and 12% and has not any predilection to side, age, and gender. However, the rate of AMF varies among different ethnic groups. For example it is 2.6% in French, 1.4% in White Americans, 5.7% in Black Americans, 1.5% in Asian-Indians, 9.0% in Pre-Columbian Nazca Indians, 3.3% in Greeks, 1.5% in Russians, 3.0% in Hungarians, 9.7% in Melanesians, 6.3% in Turkish, 8.4% in Indians, 3.6% in Egyptians, and 6.7%-12.5% in Japanese [6, 7, 9, 13, 15-18]. In this study, the incidence of AMF was 7.7%. Like other studies, no age and gender predilections were seen in the presence of AMF in this study [6, 17].
Avni Balcioglu et al. concluded that non-Caucasians might have a higher rate of AMF than Caucasians, which seemed to be in contrast with the present study [13]. Although most Iranians are Caucasian, they have shown a high prevalence of AMF similar to Japanese people. However, more studies with larger sample sizes are required to show its real incidence in Iranian population. Therefore, the sample size is as one of the limitations of this study. In another study on an Iranian population with fewer samples, the incidence of AMF is 5.1% which is similar to the present study; there were no gender and age predilections in the presence of AMF [11].
The most outstanding and novel feature in the present study, in contrast with Khojastepoor et al. study, was the classification of AMF position into eight regions [11]. Moreover, in the present study, the method of defining AMF is more accurate because of using cross-sectional images in combination with tangential and 3D images Figures 1, 2, 3. Khojastepoor et al. conducted their study on fewer samples, and did not examine the presence of AMF on the right and left sides [11].
The location of the AMF plays an important role in implant surgical procedures. Torres believed that AMF would pose no problem if it were located inferior to the mental foramen [2]. Some studies have reported that the posterior position is the most frequent location of AMF with respect to the mental foramen [2, 17, 19]. Patil et al. assessed the distribution of accessory foramen on lingual and buccal aspects of the mandible on CT images and reported a higher frequency of posterior than anterior position [20]. Our study is somehow different from the above-mentioned studies because nearly all of the eight positions were investigated in our study. Although the posterior-superior position has the most frequency out of different AMF positions, it shows the importance of pre-operation imaging examinations to identify this variation to avoid damaging of neurovascular bundles.
The prevalence of AMFs on CBCT images in a population of Indians in P. Jaju et al. study was 8.4%, and the three reported locations were posterior-inferior, anterior-inferior, and posterior-superior [9]. In our study, nearly all of the eight positions were investigated, and unlike P. Jaju et al. study, there was a difference in the frequency of AMF between the right and left sides, which might be because of the differences in the number of samples. Gershenson et al. reported that 4.3% of the studied cases had two, 0.7% had three, and one case had four mental foramina on one side. In our study, one image sample had two AMFs [21].
5. Conclusion
According to this study, there were variations in the incidence and location of the AMF so CBCT would be an effective tool for 3D pre-operation assessment of AMF. It is recommended that further similar studies be conducted with higher sample sizes and in different ethnic groups.
Ethical Considerations
Compliance with ethical guidelines
There was no ethical considerations to be considered in this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contribution's
All authors contributed in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
The prevalence of AMFs on CBCT images in a population of Indians in P. Jaju et al. study was 8.4%, and the three reported locations were posterior-inferior, anterior-inferior, and posterior-superior [9]. In our study, nearly all of the eight positions were investigated, and unlike P. Jaju et al. study, there was a difference in the frequency of AMF between the right and left sides, which might be because of the differences in the number of samples. Gershenson et al. reported that 4.3% of the studied cases had two, 0.7% had three, and one case had four mental foramina on one side. In our study, one image sample had two AMFs [21].
5. Conclusion
According to this study, there were variations in the incidence and location of the AMF so CBCT would be an effective tool for 3D pre-operation assessment of AMF. It is recommended that further similar studies be conducted with higher sample sizes and in different ethnic groups.
Ethical Considerations
Compliance with ethical guidelines
There was no ethical considerations to be considered in this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contribution's
All authors contributed in preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Sheikhi M, Karbasi Kheir M, Hekmatian E. Cone-beam computed tomography evaluation of mental foramen variations: A preliminary study. Radiology Research and Practice. 2015; 2015:124635. [DOI:10.1155/2015/124635] [PMID] [PMCID]
- Torres MG, Valverde LD, Vidal MT, Crusoé-Rebello IM. Accessory mental foramen: A rare anatomical variation detected by cone-beam computed tomography. Imaging Science in Dentistry. 2015; 45(1):61-5. [DOI:10.5624/isd.2015.45.1.61] [PMID] [PMCID]
- Arquez HF. Accessory nerve and mental foramen. International Journal of Pharma and Bio Sciences. 2014; 5(4):739-44.
- Sheikhi M, Karbasi Kheir M. CBCT assessment of mental foramen position relative to anatomical landmarks. International Journal of Dentistry. 2016; 5821048. [DOI: 10.1155/2016/5821048] [PMID] [PMCID]
- Hasan T. Mental foramen morphology: A must know in clinical dentistry. Journal of the Pakistan Dental Association. 2012; 21(3):168-73.
- Toh H, Kodama J, Yanagisako M, Ohmori T. Anatomical study of the accessory mental foramen and the distribution of its nerve. Okajimas folia anatomica Japonica. 1992; 69(2-3):85-8. [PMID]
- Göregen M, Miloğlu Ö, Ersoy İ, Şevki Bayrakdar İ, Murat Akgül H. The assessment of accessory mental foramina using cone-beam computed tomography. Turkish Journal of Medical Sciences. 2013; 43(3):479-83. [DOI:10.3906/sag-1206-105]
- Mihaylova H. Triple mental foramina detected by CBCT. International Journal of Science and Research (IJSR). 2015; 4(2):639-41.
- Jaju PP, Jaju SP, Garcha V. Accessory mental foramina detection by cone beam Ct in Indian population. Smile Dental Journal. 2013; 8(3):32-6.
- Iwanaga J, Tsuyoshi S, Tabira Y, Nakamura M, Kitashima S, Watanabe K, et al. The clinical anatomy of accessory mental nerves and foramina. Clinical Anatomy. 2015; 28(7):848-56. [DOI:10.1002/ca.22597] [PMID]
- Khojastepour L, Mirbeigi S, Mirhadi S, Safaee A. Location of mental foramen in a selected Iranian population: A CBCT assessment. Iranian Endodontic Journal. 2015; 10: 117-21. [PMID] [PMCID]
- Ahmed S, Jasani V, Ali A, Avery C. Double accessory mental foramina: Report of an anatomical variant. Oral Surgery. 2015; 8(1):51-3. [DOI:10.1111/ors.12119]
- Avni Balcioglu H, Kocaelli H. Accessory mental foramen. North American Journal of Medical Sciences. 2009; 1(6):314-5. [PMID] [PMCID]
- Mamatha NS, Kedarnath NS, Madhumathi S, Gourav P. Accessory mental nerve: A case report. Journal of Clinical and Diagnostic Research. 2013; 7(9):2078-79. [DOI:10.7860/JCDR/2013/5968.3411] [PMID] [PMCID]
- Udhaya K, Saraladevi KV, Sridhar J. The morphometric analysis of the mental foramen in adult dry human mandibles: A study on the south Indian population. Journal of Clinical and Diagnostic Research (JCDR). 2013; 7(8):1547-51. [DOI:10.7860/JCDR/2013/6060.3207] [PMID] [PMCID]
- Ramadhan A, Messo E, Hirsch JM. Anatomical variation of mental foramen: A case report. Stomatologija. 2010; 12(3):93-6. [PMID]
- Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2009; 107(2):289–94. [DOI:10.1016/j.tripleo.2008.09.010] [PMID]
- Sawyer DR, Kiely ML, Pyle MA. The frequency of accessory mental foramina in four ethnic groups. Archives of Oral Biology. 1998; 43(5):417-20. [DOI.org/10.1016/S0003-9969(98)00012-0] [PMID]
- Katakami K, Mishima A, Shiozaki K, Shimoda S, Hamada Y, Kobayashi K. Characteristics of accessory mental foramina observed on limited cone-beam computed tomography images. Journal of Endodontics. 2008; 34(12):1441-5. [DOI:10.1016/j.joen.2008.08.033] [PMID]
- Patil S, Matsuda Y, Okano T. Accessory mandibular foramina: A CT study of 300 cases. Surgical and Radiologic Anatomy (SRA). 2013; 35(4):323-30. [DOI:10.1007/s00276-012-1044-6] [PMID]
- Gershenson A, Nathan H, Luchansky E. Mental foramen and mental nerve: Changes with age. Acta Anatomica (Basel). 1986; 126(1):21-8. [DOI:10.1159/000146181] [PMID]
Type of Study: Original article |
Subject:
Radiology
Received: 2017/12/9 | Accepted: 2018/06/23 | Published: 2018/09/1
Received: 2017/12/9 | Accepted: 2018/06/23 | Published: 2018/09/1
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





.jpg)