Wed, Apr 24, 2024
Volume 7, Issue 1 (3-2018)
2018, 7(1): 23-28 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jahandideh Y, Basirat M, Kananian B. Risk Factors for Temporomandibular Joint Disorder in Dental Students. Journal title 2018; 7 (1) :23-28
URL: http://3dj.gums.ac.ir/article-1-306-en.html
URL: http://3dj.gums.ac.ir/article-1-306-en.html
1- Assistant Professor, Dental Sciences Research Center, Department of Prosthodontics, Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
2- Assistant Professor, Dental Sciences Research Center, Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. , mbasirat2010@gmail.com
3- Assistant Professor, Dental Sciences Research Center, Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
2- Assistant Professor, Dental Sciences Research Center, Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. , mbasirat2010@gmail.com
3- Assistant Professor, Dental Sciences Research Center, Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
Full-Text [PDF 621 kb]
(707 Downloads)
| Abstract (HTML) (3566 Views)
Full-Text: (1087 Views)
1. Introduction
Temporomandibular joint is one of the most used joints in the human body and plays an important role in normal oral function. Temporomandibular joint Disorder (TMD) is one of the most common disorders in the maxillofacial area and its prevalence has been reported differently in various populations [1]. TMD includes dysfunction in temporomandibular joint, masticatory muscles and involvement of some structures associated with these areas [1, 2]. TMD usually occurs as oral and facial pain, masticatory muscles tenderness (by touching the muscle or the act of chewing, yawning or clenching teeth), joint sounds (clicking or crepitus), and reduction in jaw function. Other symptoms of TMD include headache, dizziness, nausea, blurred vision, itching, tinnitus, increased stress levels, and reduced quality of life [3].
The etiology of TMD is unclear, but several causes are implicated in this problem [1, 4]. Various factors are involved in the development of TMD, which are categorized as initiating, continuing, and predisposing factors. The main initiating factors are trauma and pressure to the masticatory system. Continuing factors include behavioral factors (teeth grinding and wrong position of the head), social factors (manner of perception and response to pain), emotional factors (depression and aggression), and cognitive factors (negative thoughts that can make the disease more complicated). Predisposing factors include pathophysiological, psychological, and physical factors [2, 5, 6].
Gelb believed that TMD diagnosis is based on the presence of three factors; predisposing factors, tissue alterations, and psychological factors [2, 5]. About 70% to 84% of patients with TMD report a history of trauma [6, 7]. According to various studies, the prevalence of TMD in the world and among the Iranian population has been reported as 10% to 91%, and these disorders in women aged 20-40 years is 1.5 to 2 times more than men [7-9]. Some studies have shown that 50% to 60% of the population have experienced at least one of the symptoms of TMD [10-12]; however, patients usually do not call for treatment because the symptoms are not severe [1, 2, 10, 13].
The prevalence, causes, predisposing factors, and clinical signs and symptoms of TMD differ with respect to age, race, geographical location and time of the study in various populations. Determining the most common TMD signs and symptoms can be helpful in training people to avoid this problem. In addition, with the proper knowledge of its clinical symptoms, we can differentiate TMD pains from other types of pain like headache, earache, and other forms of neurological pains. Then, we can choose the best treatment and know the associated factors in correct diagnosis. By controlling and reducing these factors, we can reduce costly treatment and its complications. The present study aimed to investigate the prevalence of TMD among dental students of Guilan University of Medical Sciences.
2. Materials and Methods
In this descriptive and cross-sectional study, 125 dental students (from 140 students) of Post Basic Science from Guilan University of Medical Sciences agreed to participate in the study in 2016. Five uncompleted data collection forms were excluded from the study. The study data were collected through interview, observation, and clinical examination. Patients’ demographic characteristics (age, sex, education, nutrition status), clinical signs and symptoms (click, joint pain, mouth deviation during mouth opening, temporomandibular joint dislocation, loss of posterior teeth, tooth wear, and fracture of tooth restoration, hypertrophy of masticatory muscles, scalloping appearance on the lateral margins of the tongue, masticatory muscle fatigue), parafunctional habits (bruxism, clenching of the teeth), history of trauma, anxiety and depression were recorded in data forms.
The extraoral examination was performed using dental mirrors on dental unit for intraoral examination. Temporal muscle, masseter muscle, internal and external pterygoid were touched. Experiencing of any pain by the patient was recorded in special forms. Joint sounds were evaluated by putting fingertips on the outer surface of the joint in front of the tragus during mouth opening and closing. If the sound was crackling or popping, it would be considered as crepitus and recorded in the information form. Deviation of jaw was recorded as two forms; deviation (any shift of the jaw from midline during opening that disappears with continued opening) and deflection (any shift from the midline to one side that becomes greater with opening and does not disappear at maximum opening).
Joint tenderness was recorded in three states of closed mouth, during opening and closing the mouth, and opened mouth. For this purpose, the dentist passed his finger into the space behind the condyle prominence and touched this area. To evaluate the limitation of opening the mouth, the distance between the incisal edges of the maxillary and mandibular central incisors of the patient during maximum mouth opening were measured and recorded. Less than 40 mm was considered as a limitation in opening the mouth.
In intraoral examination, any unwanted contacts on balancing side was evaluated by examination of mandibular movement in maximum intercuspation state to tip state of canine teeth in left or right. If teeth in balancing side showed contact toward this movement, it would be recorded as interference of balancing side, in individual questionnaire. Dentist’s evaluation was conducted by testing the ability of passing or not passing of dental floss in balancing side, also missing teeth were assessed and recorded. The criteria for diagnosis of TMD was considered as existence of at least one of disorders, including pain in temporomandibular joint area, joint, sound during moving, tenderness of masticatory muscles, jaw deviation, and limited mouth opening.
The obtained data were analyzed by using SPSS version 17. The descriptive statistics of the results, including frequency and percentage were presented. The impact of factors affecting the prevalence of TMD was evaluated using the Chi-square and Pearson correlation coefficient. In this study, statistical significance value was considered as P<0.05.
3. Results
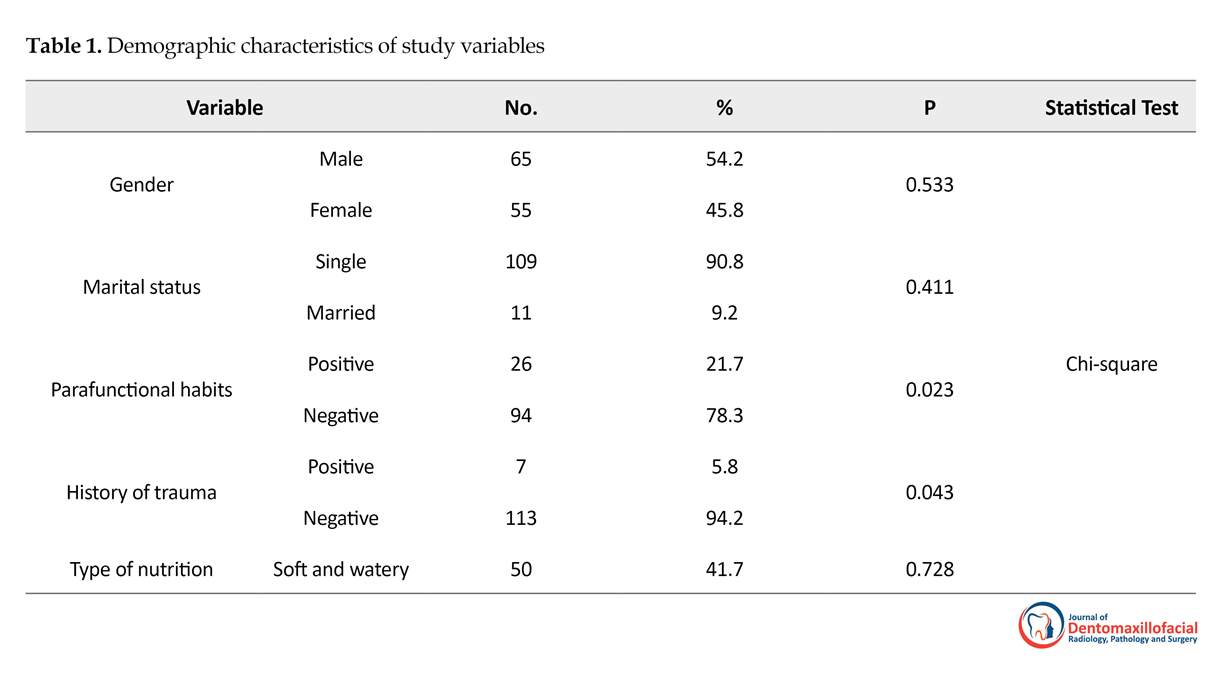
Out of 120 dental students participated in the study, 55 (45.8%) were women and 65 (54.2%) were men. The 109 (90.8%) subjects were single and 11 (9.2%) were married. Their Mean±SD age was 23.50±2.97 years (Table 1). The most common symptoms of TMD were clicking of joint one or two sides (28.4%), jaw deviation when opening the mouth (20%), limitations in opening the mouth (13.3%), pain in the jaw joint (10.8%), and masseter muscles tenderness (10%) (Table 2).
According to Tables 1 and 2, there was a significant relation between parafunctional habits (P=0.023), history of trauma (P=0.034), pain on temporomandibular joint (P=0.002) muscle tenderness (P=0.002), tooth wear (P=0.006), limitation in jaw opening (P=0.002), jaw dislocation (P=0.034), and TMD.
There were not relationship between TMD and variables of gender, marital status, and type of nutrition. However, there was a relationship between limitation of jaw opening and gender of students (P=0.002). There were not significant relationship between other sign and symptoms of TMDs and gender of students. There was correlation between parafunctional habits (P=0.000, r=-0.364) and also muscle tenderness (P=0.045, r=-0.314) and age of students based on Spearman correlation test.
4. Discussion
In this study, 120 patients aged 20 to 27 years were evaluated based on diagnostic criteria of TMD; the prevalence of TMD was found 28%. The results of this study were consistent with Lasemi et al. [7], Soukaini et al. [13] studies although these results were inconsistent with Kitsoulis [14] and Hegde studies [15]. It can be due to different sample size, race, and culture.
Temporomandibular joint is one of the most used joints in the human body and plays an important role in normal oral function. Temporomandibular joint Disorder (TMD) is one of the most common disorders in the maxillofacial area and its prevalence has been reported differently in various populations [1]. TMD includes dysfunction in temporomandibular joint, masticatory muscles and involvement of some structures associated with these areas [1, 2]. TMD usually occurs as oral and facial pain, masticatory muscles tenderness (by touching the muscle or the act of chewing, yawning or clenching teeth), joint sounds (clicking or crepitus), and reduction in jaw function. Other symptoms of TMD include headache, dizziness, nausea, blurred vision, itching, tinnitus, increased stress levels, and reduced quality of life [3].
The etiology of TMD is unclear, but several causes are implicated in this problem [1, 4]. Various factors are involved in the development of TMD, which are categorized as initiating, continuing, and predisposing factors. The main initiating factors are trauma and pressure to the masticatory system. Continuing factors include behavioral factors (teeth grinding and wrong position of the head), social factors (manner of perception and response to pain), emotional factors (depression and aggression), and cognitive factors (negative thoughts that can make the disease more complicated). Predisposing factors include pathophysiological, psychological, and physical factors [2, 5, 6].
Gelb believed that TMD diagnosis is based on the presence of three factors; predisposing factors, tissue alterations, and psychological factors [2, 5]. About 70% to 84% of patients with TMD report a history of trauma [6, 7]. According to various studies, the prevalence of TMD in the world and among the Iranian population has been reported as 10% to 91%, and these disorders in women aged 20-40 years is 1.5 to 2 times more than men [7-9]. Some studies have shown that 50% to 60% of the population have experienced at least one of the symptoms of TMD [10-12]; however, patients usually do not call for treatment because the symptoms are not severe [1, 2, 10, 13].
The prevalence, causes, predisposing factors, and clinical signs and symptoms of TMD differ with respect to age, race, geographical location and time of the study in various populations. Determining the most common TMD signs and symptoms can be helpful in training people to avoid this problem. In addition, with the proper knowledge of its clinical symptoms, we can differentiate TMD pains from other types of pain like headache, earache, and other forms of neurological pains. Then, we can choose the best treatment and know the associated factors in correct diagnosis. By controlling and reducing these factors, we can reduce costly treatment and its complications. The present study aimed to investigate the prevalence of TMD among dental students of Guilan University of Medical Sciences.
2. Materials and Methods
In this descriptive and cross-sectional study, 125 dental students (from 140 students) of Post Basic Science from Guilan University of Medical Sciences agreed to participate in the study in 2016. Five uncompleted data collection forms were excluded from the study. The study data were collected through interview, observation, and clinical examination. Patients’ demographic characteristics (age, sex, education, nutrition status), clinical signs and symptoms (click, joint pain, mouth deviation during mouth opening, temporomandibular joint dislocation, loss of posterior teeth, tooth wear, and fracture of tooth restoration, hypertrophy of masticatory muscles, scalloping appearance on the lateral margins of the tongue, masticatory muscle fatigue), parafunctional habits (bruxism, clenching of the teeth), history of trauma, anxiety and depression were recorded in data forms.
The extraoral examination was performed using dental mirrors on dental unit for intraoral examination. Temporal muscle, masseter muscle, internal and external pterygoid were touched. Experiencing of any pain by the patient was recorded in special forms. Joint sounds were evaluated by putting fingertips on the outer surface of the joint in front of the tragus during mouth opening and closing. If the sound was crackling or popping, it would be considered as crepitus and recorded in the information form. Deviation of jaw was recorded as two forms; deviation (any shift of the jaw from midline during opening that disappears with continued opening) and deflection (any shift from the midline to one side that becomes greater with opening and does not disappear at maximum opening).
Joint tenderness was recorded in three states of closed mouth, during opening and closing the mouth, and opened mouth. For this purpose, the dentist passed his finger into the space behind the condyle prominence and touched this area. To evaluate the limitation of opening the mouth, the distance between the incisal edges of the maxillary and mandibular central incisors of the patient during maximum mouth opening were measured and recorded. Less than 40 mm was considered as a limitation in opening the mouth.
In intraoral examination, any unwanted contacts on balancing side was evaluated by examination of mandibular movement in maximum intercuspation state to tip state of canine teeth in left or right. If teeth in balancing side showed contact toward this movement, it would be recorded as interference of balancing side, in individual questionnaire. Dentist’s evaluation was conducted by testing the ability of passing or not passing of dental floss in balancing side, also missing teeth were assessed and recorded. The criteria for diagnosis of TMD was considered as existence of at least one of disorders, including pain in temporomandibular joint area, joint, sound during moving, tenderness of masticatory muscles, jaw deviation, and limited mouth opening.
The obtained data were analyzed by using SPSS version 17. The descriptive statistics of the results, including frequency and percentage were presented. The impact of factors affecting the prevalence of TMD was evaluated using the Chi-square and Pearson correlation coefficient. In this study, statistical significance value was considered as P<0.05.
3. Results
Out of 120 dental students participated in the study, 55 (45.8%) were women and 65 (54.2%) were men. The 109 (90.8%) subjects were single and 11 (9.2%) were married. Their Mean±SD age was 23.50±2.97 years (Table 1). The most common symptoms of TMD were clicking of joint one or two sides (28.4%), jaw deviation when opening the mouth (20%), limitations in opening the mouth (13.3%), pain in the jaw joint (10.8%), and masseter muscles tenderness (10%) (Table 2).
According to Tables 1 and 2, there was a significant relation between parafunctional habits (P=0.023), history of trauma (P=0.034), pain on temporomandibular joint (P=0.002) muscle tenderness (P=0.002), tooth wear (P=0.006), limitation in jaw opening (P=0.002), jaw dislocation (P=0.034), and TMD.
There were not relationship between TMD and variables of gender, marital status, and type of nutrition. However, there was a relationship between limitation of jaw opening and gender of students (P=0.002). There were not significant relationship between other sign and symptoms of TMDs and gender of students. There was correlation between parafunctional habits (P=0.000, r=-0.364) and also muscle tenderness (P=0.045, r=-0.314) and age of students based on Spearman correlation test.
4. Discussion
In this study, 120 patients aged 20 to 27 years were evaluated based on diagnostic criteria of TMD; the prevalence of TMD was found 28%. The results of this study were consistent with Lasemi et al. [7], Soukaini et al. [13] studies although these results were inconsistent with Kitsoulis [14] and Hegde studies [15]. It can be due to different sample size, race, and culture.
In the present study, the most common symptoms of TMD were clicking of joint, jaw deviation, limitations in mouth opening, pain in the jaw joint, and masseter muscle tenderness. Similar results were reported in some studies. Goharian and Madani [16] and Mahshid et al. [17] also reported the most common symptoms of TMD as joint sound, tenderness, and pain in the masticatory muscles, respectively. Sahebi and Bastani Amleshi [18] also reported that joint sound, masticatory muscle tenderness, and joint pain in mixed dentition are more common.
In the present study, there was a significant relation between parafunctional habits (P=0.023), history of trauma (P=0.034), pain on temporomandibular joint (P=0.002), muscle tenderness (P=0.002), tooth wear (P=0.006), limitation in jaw opening (P=0.002), jaw dislocation (P=0.034), and TMD. Regarding parafunctional habits, the results are consistent with Jahandideh [19], Johansson [20], Hegde [15], and Lasemi [7] studies. Regarding the history of trauma, similar results were reported in Lasemi [7] and Jahandideh [19] and Kamisaka [21] studies. The history of trauma has a significant effect on the longevity of TMD related problems [21]. Regarding tooth wear, the results were consistent with Jahandideh study [19]. Limitation in jaw opening and jaw dislocation can be created as the result of stress and TMD [22].
In this study, there were not relationship between gender, marital status and also the type of nutrition with TMD. There was relationship between limitation of jaw opening and gender of students (P=0.002). There were not significant relationship between other sign and symptoms of TMD and gender of students. In this regard, Jahandideh et al. found no statistically significant relationship between sex and TMD [19]. However, in most studies, the incidence of TMD in women is higher than men [10]. Inconsistent with our study, Kitsoulis et al. [14] and Shetty [10] reported that the incidence or severity of TMD is more common in women than men. Also, Lasmi et al. found that sex is an effective factor in the prevalence of TMD [7].
In most studies, the high prevalence of TMD in women has been attributed to high levels of stress in women, which needs further investigation. Similar to this study, Bruno study [23] indicate that marital status is incorporated into myofascial pain. Type of nutrition should also be investigated more in future research studies.
5. Conclusion
TMD is a relatively common condition among dental students. Based on the finding of this study, the prevalence of TMD is directly related with factors such as parafunctional habits, tooth wear, jaw dislocation, trauma, and in some symptoms with age. However, the risk of TMD is not related to the factors such as gender, nutrition, headache, migraine, marital status, earache, loss of posterior teeth, and contact in balancing side. By providing the necessary training for students, especially for those who are at risk (those with parafunctional habits, tooth wear, jaw dislocation, trauma), we can prevent TMD. In addition, it is suggested that the prevalence of TMD be investigated in normal population.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Ethical Committee of Guilan University of Medical Sciences. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Concept, design, acquisition of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content and analysis and interpretation of the data: Yosef Jahandideh and Maryam Basirat; and responsible for the administrative, technical, and material support: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Zahra Pourhabibi for performing statistical analysis and all of participants for her help in this research.
Reference
In the present study, there was a significant relation between parafunctional habits (P=0.023), history of trauma (P=0.034), pain on temporomandibular joint (P=0.002), muscle tenderness (P=0.002), tooth wear (P=0.006), limitation in jaw opening (P=0.002), jaw dislocation (P=0.034), and TMD. Regarding parafunctional habits, the results are consistent with Jahandideh [19], Johansson [20], Hegde [15], and Lasemi [7] studies. Regarding the history of trauma, similar results were reported in Lasemi [7] and Jahandideh [19] and Kamisaka [21] studies. The history of trauma has a significant effect on the longevity of TMD related problems [21]. Regarding tooth wear, the results were consistent with Jahandideh study [19]. Limitation in jaw opening and jaw dislocation can be created as the result of stress and TMD [22].
In this study, there were not relationship between gender, marital status and also the type of nutrition with TMD. There was relationship between limitation of jaw opening and gender of students (P=0.002). There were not significant relationship between other sign and symptoms of TMD and gender of students. In this regard, Jahandideh et al. found no statistically significant relationship between sex and TMD [19]. However, in most studies, the incidence of TMD in women is higher than men [10]. Inconsistent with our study, Kitsoulis et al. [14] and Shetty [10] reported that the incidence or severity of TMD is more common in women than men. Also, Lasmi et al. found that sex is an effective factor in the prevalence of TMD [7].
In most studies, the high prevalence of TMD in women has been attributed to high levels of stress in women, which needs further investigation. Similar to this study, Bruno study [23] indicate that marital status is incorporated into myofascial pain. Type of nutrition should also be investigated more in future research studies.
5. Conclusion
TMD is a relatively common condition among dental students. Based on the finding of this study, the prevalence of TMD is directly related with factors such as parafunctional habits, tooth wear, jaw dislocation, trauma, and in some symptoms with age. However, the risk of TMD is not related to the factors such as gender, nutrition, headache, migraine, marital status, earache, loss of posterior teeth, and contact in balancing side. By providing the necessary training for students, especially for those who are at risk (those with parafunctional habits, tooth wear, jaw dislocation, trauma), we can prevent TMD. In addition, it is suggested that the prevalence of TMD be investigated in normal population.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by Ethical Committee of Guilan University of Medical Sciences. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors contributions
Concept, design, acquisition of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content and analysis and interpretation of the data: Yosef Jahandideh and Maryam Basirat; and responsible for the administrative, technical, and material support: All authors.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank Zahra Pourhabibi for performing statistical analysis and all of participants for her help in this research.
Reference
- De Rossi SS, Greenberg MS, Liu F, Steinkeler A. Temporomandibular disorders: Evaluation and management. Medical Clinics. 2014; 98(6):1353-84. [DOI:10.1016/j.mcna.2014.08.009] [PMID]
- Sharma S, Gupta DS, Pal U, Jurel SK. Etiological factors of temporomandibular joint disorders. National Journal of Maxillofacial Surgery. 2011; 2(2):116-9. [DOI:10.4103/0975-5950.94463] [PMID] [PMCID]
- Suma S, Kumar BV. Temporomandibular disorders and functional somatic syndromes: Deliberations for the dentist. Indian Journal of Dental Research. 2012; 23(4):529-36. [DOI:10.4103/0970-9290.104965] [PMID]
- Calixtre LB, Gruninger BLdS, Chaves TC, Oliveira ABd. Is there an association between anxiety/depression and temporomandibular disorders in college students? Journal of Applied Oral Science. 2014; 22(1):15-21. [DOI:10.1590/1678-775720130054] [PMID] [PMCID]
- Eslamian L, Alizadehagha F. [Epidemiology of temporomandibular joint disorders in dental students at Shahid Beheshti University 1999 (Persian)]. Journal of Dental School Shahid Beheshti University of Medical Science. 2001; 19(1):25-31.
- Häggman Henrikson B, Rezvani M, List T. Prevalence of whiplash trauma in TMD patients: A systematic review. Journal of Oral Rehabilitation. 2014; 41(1):59-68. [DOI:10.1111/joor.12123] [PMID]
- Lasemi E, Navi F, Basir Shabastari S. [Prevalence of temporomandibular disorders and it’s related factors in dental school of Azad University of Tehran in 2005 (Persian)]. Journal of Mashhad Dental School. 2008; 32(1):59-64.
- Ebrahimi M DH, Mehrabkhani M, Arghavani M, Daneshvar Mozafari A. Temporomandibular disorders and related factors in a group of Iranian adolescents: A cross-sectional survey. Journal of Dental Research, Dental Clinics, Dental Prospects. 2011; 5(4):123-7. [PMCID]
- Bahrani F, Ghadiri P, Vojdani M. Comparison of temporomandibular disorders in Iranian dental and nondental students. The Journal of Contemporary Dental Practice. 2012; 13(2):173-7. [DOI:10.5005/jp-journals-10024-1116]
- Shetty R. Prevalence of signs of temporomandibular joint dysfunction in asymptomatic edentulous subjects: A cross-sectional study. The Journal of Indian Prosthodontic Society. 2010; 10(2):96-101. [DOI:10.1007/s13191-010-0018-9] [PMID] [PMCID]
- Akhter R, Morita M, Ekuni D, Hassan NMM, Furuta M, Yamanaka R, et al. Self-reported aural symptoms, headache and temporomandibular disorders in Japanese young adults. BMC Musculoskeletal Disorders. 2013; 14:58. [DOI:10.1186/1471-2474-14-58] [PMID] [PMCID]
- Sánchez Pérez L, Irigoyen Camacho ME, Molina Frechero N, Mendoza Roaf P, Medina Solís C, Acosta Gío E, et al. Malocclusion and TMJ disorders in teenagers from private and public schools in Mexico city. Medicina Oral, Patología Oral y Cirugía Bucal. 2013; 18(2):e312-e8. [DOI:10.4317/medoral.18075] [PMID] [PMCID]
- Ryalat S, Baqain ZH, Amin WM, Sawair F, Samara O, Badran DH. Prevalence of temporomandibular joint disorders among students of the University of Jordan. Journal of Clinical Medicine Research. 2009; 1(3):158-64. [DOI:10.4021/jocmr2009.06.1245]
- Kitsoulis P, Marini A, Iliou K, Galani V, Zimpis A, Kanavaros P, et al. Signs and symptoms of temporomandibular joint disorders related to the degree of mouth opening and hearing loss. BMC Ear, Nose and Throat Disorders. 2011; 11:5. [DOI:10.1186/1472-6815-11-5] [PMID] [PMCID]
- Hegde S, Mahadev R, Ganapathy K, Sujatha D, Patil BA. Prevalence of signs and symptoms of temporomandibular disorders in dental students. Journal of Indian Academy of Oral Medicine and Radiology. 2011; 23(5):316-9. [DOI:10.5005/jp-journals-10011-1158]
- Gouharian R, Madani AA. [Evaluation of temporomandibular joint status and related signs and symptoms in students of Mashhad Dental School (Persian)]. Iranian Journal of Otorhinolaryngology. 2006; 17(4):197-202.
- Mahshid M, Ejlali M, Nouri M, Drodian AA, Shalchizadeh A. [Prevalence of temporomandibular disorders in clinics and health centers in Tehran during summer 2001 (Persian)]. Shahid Beheshti University Dental Journal. 2007; 25(2):200-8.
- Sahebi M, Bostani Amlashi P. [Prevalence of temporomandibular disorders and its association with malocclusion in mixed dentition among patients referred to Tehran Dental School (Persian)]. Journal of Dental Medicine. 2010; 23(3):153-60.
- Jahandideh Y, Hasan NH, Basirat M, Tayefeh DR. [Prevalence of temporomandibular disorders and the associated factors (Persian)]. Journal of Guilan University of Medical Sciences. 2017; 26(103):22-29.
- Johansson A, Unell L, Carlsson GE, Söderfeldt B, Halling A. Differences in four reported symptoms related to temporomandibular disorders in a cohort of 50-year-old subjects followed up after 10 years. Acta Odontologica Scandinavica. 2008; 66(1):50-7. [DOI:10.1080/00016350801922775] [PMID]
- Kamisaka M, Yatani H, Kuboki T, Matsuka Y, Minakuchi H. Four-year longitudinal course of TMD symptoms in an adult population and the estimation of risk factors in relation to symptoms. Journal of Orofacial Pain. 2000; 14(3):224-32. [PMID]
- Choi YS, Choung PH, Moon HS, Kim SG. Temporomandibular disorders in 19-year-old Korean men. Journal of Oral and Maxillofacial Surgery. 2002; 60(7):797-803. [DOI:10.1053/joms.2002.33249]
- Magalhães BG, de Sousa ST, de Mello VVC, da Silva Barbosa AC, de Assis Morais MPL, Barbosa Vasconcelos MMV, et al. Risk factors for temporomandibular disorder: Binary logistic regression analysis. Medicina Oral, Patologia Oral Cirugia Bucal. 2014; 19(3):e232-6. [DOI:10.4317/medoral.19434] [PMID] [PMCID]
Type of Study: Original article |
Subject:
Pathology
Received: 2018/08/10 | Accepted: 2017/12/23 | Published: 2018/03/1
Received: 2018/08/10 | Accepted: 2017/12/23 | Published: 2018/03/1
References
1. De Rossi SS, Greenberg MS, Liu F, Steinkeler A. Temporomandibular disorders: Evaluation and management. Medical Clinics. 2014; 98(6):1353-84. [DOI:10.1016/j.mcna.2014.08.009] [PMID] [DOI:10.1016/j.mcna.2014.08.009]
2. Sharma S, Gupta DS, Pal U, Jurel SK. Etiological factors of temporomandibular joint disorders. National Journal of Maxillofacial Surgery. 2011; 2(2):116-9. [DOI:10.4103/0975-5950.94463] [PMID] [PMCID] [DOI:10.4103/0975-5950.94463]
3. Suma S, Kumar BV. Temporomandibular disorders and functional somatic syndromes: Deliberations for the dentist. Indian Journal of Dental Research. 2012; 23(4):529-36. [DOI:10.4103/0970-9290.104965] [PMID] [DOI:10.4103/0970-9290.104965]
4. Calixtre LB, Gruninger BLdS, Chaves TC, Oliveira ABd. Is there an association between anxiety/depression and temporomandibular disorders in college students? Journal of Applied Oral Science. 2014; 22(1):15-21. [DOI:10.1590/1678-775720130054] [PMID] [PMCID] [DOI:10.1590/1678-775720130054]
5. Eslamian L, Alizadehagha F. [Epidemiology of temporomandibular joint disorders in dental students at Shahid Beheshti University 1999 (Persian)]. Journal of Dental School Shahid Beheshti University of Medical Science. 2001; 19(1):25-31.
6. Häggman Henrikson B, Rezvani M, List T. Prevalence of whiplash trauma in TMD patients: A systematic review. Journal of Oral Rehabilitation. 2014; 41(1):59-68. [DOI:10.1111/joor.12123] [PMID] [DOI:10.1111/joor.12123]
7. Lasemi E, Navi F, Basir Shabastari S. [Prevalence of temporomandibular disorders and it's related factors in dental school of Azad University of Tehran in 2005 (Persian)]. Journal of Mashhad Dental School. 2008; 32(1):59-64.
8. Ebrahimi M DH, Mehrabkhani M, Arghavani M, Daneshvar Mozafari A. Temporomandibular disorders and related factors in a group of Iranian adolescents: A cross-sectional survey. Journal of Dental Research, Dental Clinics, Dental Prospects. 2011; 5(4):123-7. [PMCID] [PMCID]
9. Bahrani F, Ghadiri P, Vojdani M. Comparison of temporomandibular disorders in Iranian dental and nondental students. The Journal of Contemporary Dental Practice. 2012; 13(2):173-7. [DOI:10.5005/jp-journals-10024-1116] [DOI:10.5005/jp-journals-10024-1116]
10. Shetty R. Prevalence of signs of temporomandibular joint dysfunction in asymptomatic edentulous subjects: A cross-sectional study. The Journal of Indian Prosthodontic Society. 2010; 10(2):96-101. [DOI:10.1007/s13191-010-0018-9] [PMID] [PMCID] [DOI:10.1007/s13191-010-0018-9]
11. Akhter R, Morita M, Ekuni D, Hassan NMM, Furuta M, Yamanaka R, et al. Self-reported aural symptoms, headache and temporomandibular disorders in Japanese young adults. BMC Musculoskeletal Disorders. 2013; 14:58. [DOI:10.1186/1471-2474-14-58] [PMID] [PMCID] [DOI:10.1186/1471-2474-14-58]
12. Sánchez Pérez L, Irigoyen Camacho ME, Molina Frechero N, Mendoza Roaf P, Medina Solís C, Acosta Gío E, et al. Malocclusion and TMJ disorders in teenagers from private and public schools in Mexico city. Medicina Oral, Patología Oral y Cirugía Bucal. 2013; 18(2):e312-e8. [DOI:10.4317/medoral.18075] [PMID] [PMCID] [DOI:10.4317/medoral.18075]
13. Ryalat S, Baqain ZH, Amin WM, Sawair F, Samara O, Badran DH. Prevalence of temporomandibular joint disorders among students of the University of Jordan. Journal of Clinical Medicine Research. 2009; 1(3):158-64. [DOI:10.4021/jocmr2009.06.1245] [DOI:10.4021/jocmr2009.06.1245]
14. Kitsoulis P, Marini A, Iliou K, Galani V, Zimpis A, Kanavaros P, et al. Signs and symptoms of temporomandibular joint disorders related to the degree of mouth opening and hearing loss. BMC Ear, Nose and Throat Disorders. 2011; 11:5. [DOI:10.1186/1472-6815-11-5] [PMID] [PMCID] [DOI:10.1186/1472-6815-11-5]
15. Hegde S, Mahadev R, Ganapathy K, Sujatha D, Patil BA. Prevalence of signs and symptoms of temporomandibular disorders in dental students. Journal of Indian Academy of Oral Medicine and Radiology. 2011; 23(5):316-9. [DOI:10.5005/jp-journals-10011-1158] [DOI:10.5005/jp-journals-10011-1158]
16. Gouharian R, Madani AA. [Evaluation of temporomandibular joint status and related signs and symptoms in students of Mashhad Dental School (Persian)]. Iranian Journal of Otorhinolaryngology. 2006; 17(4):197-202.
17. Mahshid M, Ejlali M, Nouri M, Drodian AA, Shalchizadeh A. [Prevalence of temporomandibular disorders in clinics and health centers in Tehran during summer 2001 (Persian)]. Shahid Beheshti University Dental Journal. 2007; 25(2):200-8.
18. Sahebi M, Bostani Amlashi P. [Prevalence of temporomandibular disorders and its association with malocclusion in mixed dentition among patients referred to Tehran Dental School (Persian)]. Journal of Dental Medicine. 2010; 23(3):153-60.
19. Jahandideh Y, Hasan NH, Basirat M, Tayefeh DR. [Prevalence of temporomandibular disorders and the associated factors (Persian)]. Journal of Guilan University of Medical Sciences. 2017; 26(103):22-29.
20. Johansson A, Unell L, Carlsson GE, Söderfeldt B, Halling A. Differences in four reported symptoms related to temporomandibular disorders in a cohort of 50-year-old subjects followed up after 10 years. Acta Odontologica Scandinavica. 2008; 66(1):50-7. [DOI:10.1080/00016350801922775] [PMID] [DOI:10.1080/00016350801922775]
21. Kamisaka M, Yatani H, Kuboki T, Matsuka Y, Minakuchi H. Four-year longitudinal course of TMD symptoms in an adult population and the estimation of risk factors in relation to symptoms. Journal of Orofacial Pain. 2000; 14(3):224-32. [PMID] [PMID]
22. Choi YS, Choung PH, Moon HS, Kim SG. Temporomandibular disorders in 19-year-old Korean men. Journal of Oral and Maxillofacial Surgery. 2002; 60(7):797-803. [DOI:10.1053/joms.2002.33249] [DOI:10.1053/joms.2002.33249]
23. Magalhães BG, de Sousa ST, de Mello VVC, da Silva Barbosa AC, de Assis Morais MPL, Barbosa Vasconcelos MMV, et al. Risk factors for temporomandibular disorder: Binary logistic regression analysis. Medicina Oral, Patologia Oral Cirugia Bucal. 2014; 19(3):e232-6. [DOI:10.4317/medoral.19434] [PMID] [PMCID] [DOI:10.4317/medoral.19434]
Send email to the article author
| Rights and permissions | |
 | This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |